endobronchial valve placement BLVR offers nonsurgical option for COPD patients
- related: COPD chronic obstructive pulmonary disease
- tags: #literature #pulmonology
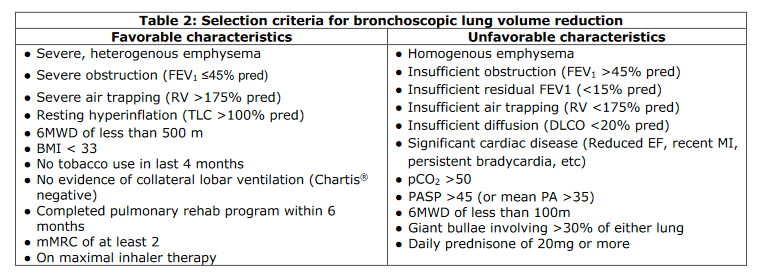
More recent explorations of BLVR with endobronchial plugs, thermal ablation, and nitinol coils have not shown consistent benefit, but endobronchial valve placement has been shown to improve FEV1, 6-min walk distance, and symptoms on the modified Medical Research Council scale and St. George’s Respiratory Questionnaire in two randomized clinical trials. Like this patient, subjects in these trials had preprocedure FEV1 less than 45% predicted, total lung capacity greater than 100% predicted, and heterogeneous emphysema. BLVR does not improve mortality.
For a successful endobronchial valve treatment, there should be little to no interlobar collateral ventilation. This is typically determined before valve placement by using either a quantitative CT scan assessment and/or an intraoperative physiologic assessment. In humans, an intact fissure is more common on the left than on the right, accounting for more successful BLVR procedures on the left lung.
Because of the intended nature of lung volume reduction, the incidence of post-BLVR pneumothorax in the two large clinical trials was 25% to 30%. Most pneumothoraces occur within the first few hours after the procedure. However, even patients with a postprocedure pneumothorax were more likely than control subjects to have long-term improvement in both lung function and respiratory symptoms.2
Hospital Stay
• Minimum of three nights with daily morning chest X-rays.
• Ambulation:
o Days 0 - 1: Limit to in-room ambulation as tolerated
o Days 2 - discharge: Ambulate in hallway 4 times dailyDischarge Day
• Perform a walk test to assess oxygen needs.
• Schedule 6-week follow-up with the pulmonologist who did the initial bLVR consult along with PFTs (spirometry, lung volumes, DLco) and a non-contrast chest CT at that time.
• Instruct patients to call for: worsening shortness of breath, cough, purulent sputum, fever, chills, hemoptysis, or chest pain.
• Activities are not restricted, but no air travel until medically cleared.
All patients should have a mandatory pulmonary consult and should be seen by the consult team daily until discharge. We aim to admit patients to the PIM service, but beds are often limited. If the patient is admitted to PIM and then is transferred out, please communicate with the consult team directly so that they can facilitate the patient’s timely discharge.
Links to this note
Footnotes
-
COPD Part III LVRS, Bipap, and Transplant ↩