euglycemic dka in DM
- related: Endocrine
- tags: #literature #endocrine
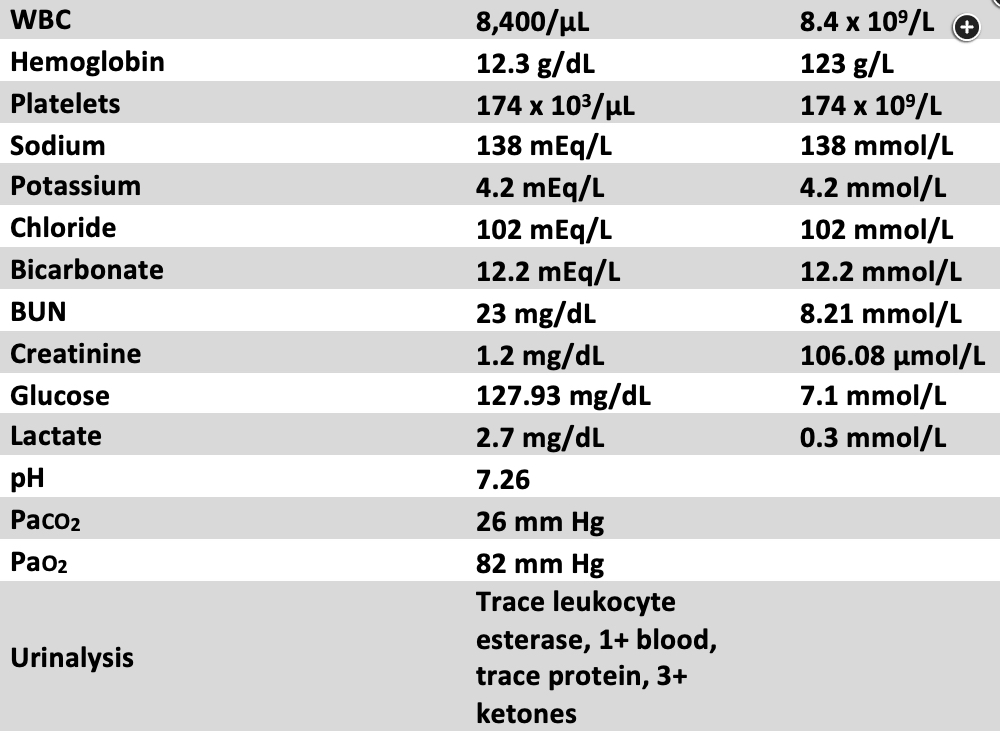
This patient’s presentation is consistent with euglycemic diabetic ketoacidosis (EDKA), as evidenced by her anion gap of 24, pH of 7.26, ketonuria, presenting symptoms of nausea and vomiting, and history of gestational diabetes. It is important to note that although ketones were detected in this patient’s urinalysis, not all commercially available urine dipstick tests detect β-hydroxybutyrate and acetoacetic acid. Thus, serum testing for ketones and/or β-hydroxybutyrate should be performed in cases in which DKA is suspected.
In EDKA, the glucose level is normal or near normal. It can be difficult to distinguish from starvation ketosis, and the two may coexist. However, in starvation ketosis, the acidosis is typically less severe, with the serum bicarbonate level and pH usually not less than 18 mEq/L (18 mmol/L) and 7.3, respectively. Management of EDKA is largely similar to that of typical DKA and includes administration of IV insulin infusion, although dextrose infusion is necessary to avoid hypoglycemia (choice C is correct). Triggers for EDKA are similar to those for typical DKA (ie, DKA with hyperglycemia) and include infection or other acute illness, new onset of diabetes, and medication noncompliance. However, risk factors for EDKA specifically include pregnancy, decreased caloric intake, and the use of sodium-glucose cotransporter-2 (SGLT-2) inhibitors. EDKA portends worse outcomes than does DKA, possibly because of delayed diagnosis in the absence of hyperglycemia. Maternal EDKA can increase the risk of both fetal demise and maternal mortality. Unexplained high anion gap metabolic acidosis in a patient with diabetes and associated risk factors should raise suspicion for EDKA. Serum ketone levels should be obtained, and other reasons for anion gap acidosis should also be ruled out.
Although pregnancy increases the risk of pulmonary embolism, the patient’s symptoms are not consistent with this diagnosis (choice A is incorrect). Furthermore, CT scanning would result in unnecessary fetal radiation exposure. Although infection should be ruled out as a precipitating factor for EDKA, the patient does not currently have any associated signs or symptoms (choice B is incorrect). The patient does not have any abdominal pain, and nausea and vomiting are likely symptoms of DKA and/or pregnancy; thus right upper quadrant ultrasonography is not currently indicated (choice D is incorrect).1234
A 35-year-old pregnant woman (gravida 2, para 1) at 8 weeks’ gestation presents to the emergency department with nausea, vomiting, and dyspnea. Her medical history is significant for obesity and well-controlled gestational diabetes (hemoglobin A1c of 6.3% [0.06]). Her vital signs include a temperature of 37.3 °C, heart rate of 114/min, BP of 98/65 mm Hg, respiratory rate of 24/min, and SpO2 of 98%. The patient appears fatigued, but physical examination results are otherwise within normal limits. Laboratory values are shown in Figure 1. She receives 2 L of isotonic IV fluids.
What is the most appropriate next step in management?
Links to this note
Footnotes
-
Chow E, Clement S, Garg R. Euglycemic diabetic ketoacidosis in the era of SGLT-2 inhibitors. BMJ Open Diabetes Res Care. 2023;11(5):e003666. PubMed ↩
-
Hamidi OP, Barbour LA. Endocrine emergencies during pregnancy: diabetic ketoacidosis and thyroid storm. Obstet Gynecol Clin North Am. 2022;49(3):473-489. PubMed ↩
-
Modi A, Agrawal A, Morgan F. Euglycemic diabetic ketoacidosis: a review. Curr Diabetes Rev. 2017;13(3):315-321. PubMed ↩