exercise induced bronchoconstriction is decrease in FEV1 after exercise
- related: PFT and lung functions, Asthma reactive airway disease
- tags: #literature #pulmonology
This patient presents with shortness of breath with exertion in the setting of normal pulmonary function and a normal methacholine challenge test. Cardiopulmonary exercise testing revealed normal performance and values, except for a 14% decrease in the FEV1 from the pre-exercise value (3.51 to 3.03 L) (Figure 5) immediately following exercise consistent with a diagnosis of exercise-induced bronchoconstriction (EIB) (choice C is correct). Exercise-associated airway narrowing occurs in most patients with asthma. Although patients often deny or do not recognize other symptoms of asthma, these symptoms can often be detected with a careful clinical history. A diagnosis of EIB is not excluded by a negative methacholine challenge test, although it is commonly positive in this clinical setting. In this instance, the patient underwent cardiopulmonary exercise testing to understand objectively the patient’s symptoms of exertional dyspnea and impaired exercise performance, which was confirmed to be normal (the patient demonstrated normal work and aerobic capacity) (Figure 2). However, spirometry following exercise (Figure 5) revealed a significant decrement in the FEV1, which subsequently responded to the administration of a bronchodilator.
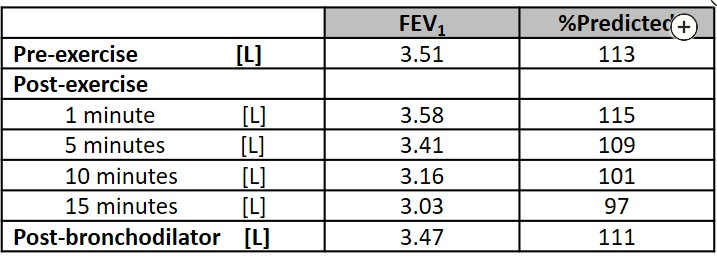
A suggested postexercise spirometry testing schedule is 1, 3, 5, 10, 15, 20, and 30 min after cessation of exercise, although if the FEV1 has returned from its nadir to the baseline level (or greater), spirometry testing may be terminated at 20 min after exercise. It is recommended to assess FEV1 because this measurement has better repeatability and is more discriminating than peak expiratory flow rate. A significant drop in FEV1 following exercise confirms the diagnosis of EIB, although if these results were not demonstrated with this incremental protocol and clinical suspicion for EIB remained, a more specific EIB exercise protocol would have been indicated. This typically consists of high-intensity exercise on a treadmill or bicycle ergometer for 6 to 8 min intended to achieve rapidly the highest possible level of ventilation for 4 to 6 min. The ventilation required for a valid test is at least 17.5 times FEV1 and preferably >21 times FEV1.There should not be a significant warm-up period, which may lead to tolerance or refractoriness to EIB, which can also occur if exercise duration exceeds 12 min (as potentially with running a half-marathon). A fall in the FEV1 of 10% or more is interpreted as abnormal. Severity may subsequently be graded as mild (>10% but <25%), moderate (>25% but <50%), or severe if the fall in FEV1 from the pre-exercise is >50%. These bronchoconstriction responses may also occasionally be demonstrated with eucapnic voluntary hyperventilation; cold air challenge; hyperosmolar aerosols, including 4.5% saline; and dry powder mannitol.
Not mentioned in the information provided is that the patient’s symptoms were also reproduced immediately following exercise; this is a common finding and helps to strengthen the diagnosis further. However, the diagnosis of EIB is established by changes in lung function provoked by exercise, not based on symptoms. A significant fall in the FEV1 may also be seen in patients with upper airway obstruction or vocal cord dysfunction, and these cases can be readily distinguished from EIB by examination of the exercise tidal flow-volume curves. In this patient, the tidal exercise flow-volume curves, both at rest and with exercise, do not reveal any changes consistent with central airway obstruction (choice A is incorrect). Patients with mitochondrial myopathies characteristically demonstrate significant aerobic and work impairment, with an early anaerobic threshold, often accompanied by an exaggerated heart rate response during exercise (choice B is incorrect). While the patient works in a stressful occupation, there are no findings consistent with primary hyperventilation syndrome, such as an erratic breathing pattern or hyperventilation that is excessive for the simultaneous metabolic load (choice D is incorrect).