fusarium infections in neutropenic patients
- related: Infectious Disease ID
- tags: #literature #id
Because of decreased susceptibility to antifungal therapy and increased use of prophylaxis with antifungal agents, mold infections are increasing in certain populations of patients who are immunocompromised. This has clinical importance with Fusarium infections because of that pathogen’s lack of predictable response to antifungal agents like echinocandins or voriconazole, which are often administered empirically in the ICU when fungal infections are suspected.
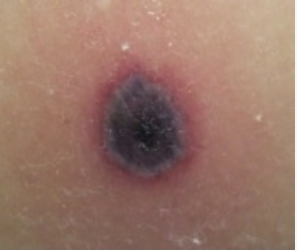
In humans, mold infection with Fusarium species manifests as a broad spectrum of disease. In the immunocompetent host, this may take the form of such superficial infections as keratitis or onychomycosis. With states of severe immunocompromise, characteristic patterns of infection are sinusitis, endophthalmitis, pneumonia, skin involvement, and fungemia. Typical of fungal infections in patients with neutropenia, infection with Fusarium usually occurs in the setting of prolonged neutropenia. Highly characteristic of the clinical presentation are positive blood cultures (which can occur in up to 40% of patients) and widely disseminated skin lesions. The lesions are characteristically reddish gray macules, some with central ulceration but others with black eschar formation, consistent with the angioinvasive property of Fusarium. The microscopic branching angle of Fusarium is similar to that of Aspergillus. The distinction between Fusarium and Aspergillus is clinically relevant because these pathogens respond differently to antifungal agents. The amphotericin B minimum inhibitory concentrations for Fusarium are usually higher than are the amphotericin minimum inhibitory concentrations for Aspergillus species. Despite the lack of complete activity, susceptibility of Fusarium to amphotericin B is usually higher than to the azoles (voriconazole, posaconazole, and isavuconazole). As a result of the limited activity of azoles against Fusarium, breakthrough infection with Fusarium is proportionately more common in patients receiving azole prophylaxis with posaconazole than are breakthrough infections with Candida or Aspergillus. Against Fusarium, the echinocandins (micafungin, caspofungin, and anidulafungin) lack clinically significant activity. As antifungal therapy, a lipid formulation of amphotericin B might be more efficacious than voriconazole (a drug of choice for Aspergillus) or an echinocandin (a drug of choice for Candida). Source control of onychomycosis is important in patients with Fusarium disseminated infection (choice B is correct).
Of the pathogenic molds in humans, Aspergillus is the most likely to mimic Fusarium clinically. In patients with neutropenia, Aspergillus has the property of angioinvasiveness, and the clinical manifestations often include evidence of infarction at the classic sites of infection: lung, sinuses, skin, and CNS. In contrast to Fusarium, Aspergillus does not commonly grow in blood cultures. When skin lesions due to Aspergillus are present in patients with neutropenia, they usually occur as a single lesion, often at a site of inoculation (such as a previous IV catheter), in contrast to the disseminated skin lesions that occur with fungemia due to Fusarium (choice A is incorrect).
Scedosporium species are molds that can act as either primary or opportunistic pathogens to cause infections in both immunocompetent and immunocompromised hosts. The spectrum of infection ranges from asymptomatic colonization of the respiratory tract, to superficial infections and allergic reactions, to severe invasive localized or disseminated fungal infections. The classic patients at risk are those who are immunocompromised, particularly with hematological malignancies. An important predisposition to infection by these pathogens is prior antifungal prophylaxis, which usually is not active against Scedosporium and, therefore, predisposes a person to clinical disease caused by it. Among individuals who are immunocompetent who can develop clinical disease are those with near-drowning events in water polluted with fungal organisms. Classic organ systems of involvement include the sinuses, lungs, and CNS. Scedosporium rarely grows in blood cultures, and skin lesions are not a classic part of the disease spectrum of these species of molds (choice C is incorrect).
Mucormycosis, caused by molds in the Mucorales family (including Rhizopus species and Mucor species), is the second most common mold infection in patients with hematological malignancy or after transplant, with mortality rates that can be >90% when infection is disseminated. Because of its propensity to use iron as an element for growth, repeated blood transfusion in patients with myelodysplastic syndrome who undergo bone marrow transplant can lead to high fatality rates caused by this mold. In addition to its siderophilic property, the agents of mucormycosis are angioinvasive, inducing blood vessel thrombosis and tissue necrosis. Blood cultures are rarely positive with this pathogen, and disseminated skin lesions are not part of the clinical picture (choice D is incorrect).12345678
Links to this note
Footnotes
-
Al-Hatmi AMS, Bonifaz A, Ranque S, et al. Current antifungal treatment of fusariosis. Int J Antimicrob Agents. 2018;51(3):326-332. PubMed ↩
-
Bodey GP, Boktour M, Mays S, et al. Skin lesions associated with Fusarium infection. J Am Acad Dermatol. 2002;47(5):659-666. PubMed ↩
-
Kosmidis C, Denning DW. The clinical spectrum of pulmonary aspergillosis. Thorax. 2015;70(3):270-277. PubMed ↩
-
Lerolle N, Raffoux E, Socie G, et al. Breakthrough invasive fungal disease in patients receiving posaconazole primary prophylaxis: a 4-year study. Clin Microbiol Infect. 2014;20(11):O952-O959. PubMed ↩
-
Mendoza L, Vilela R, Voelz K, et al. Human fungal pathogens of Mucorales and Entomophthorales. Cold Spring Harb Perspect Med. 2014;5(4):a019562. PubMed ↩
-
Muhammed M, Anagnostou T, Desalermos A, et al. Fusarium infection: report of 26 cases and review of 97 cases from the literature. Medicine (Baltimore). 2013;92(6):305-316. PubMed ↩
-
Ramirez-Garcia A, Pellon A, Rementeria A, et al. Scedosporium and Lomentospora: an updated overview of underrated opportunists. Med Mycol. 2018;56(suppl 1):102-125. PubMed ↩