GI bleed
- Keywords:: GI gastroenterology Step 3, lower GI bleed, upper GI bleed
- HALT IT trial showed TXA Did not improve mortality in GI bleed
- Hematochezia (bright red blood per rectum or maroon-colored stools) is nearly always due to lower gastrointestinal bleeding (LGIB).
- Hematemesis and melena are more common in upper GI bleeding (UGIB), although UGIB can sometimes present with hematochezia if bleeding is particularly brisk.
- Hemodynamic compromise, orthostasis, and a blood urea nitrogen-to-creatinine (BUN/Cr) ratio >20:1 are suggestive of UGIB. If the bleeding source is unclear, nasogastric lavage with aspiration of bile and absence of blood increases the likelihood of LGIB (but cannot exclude distal UGIB).
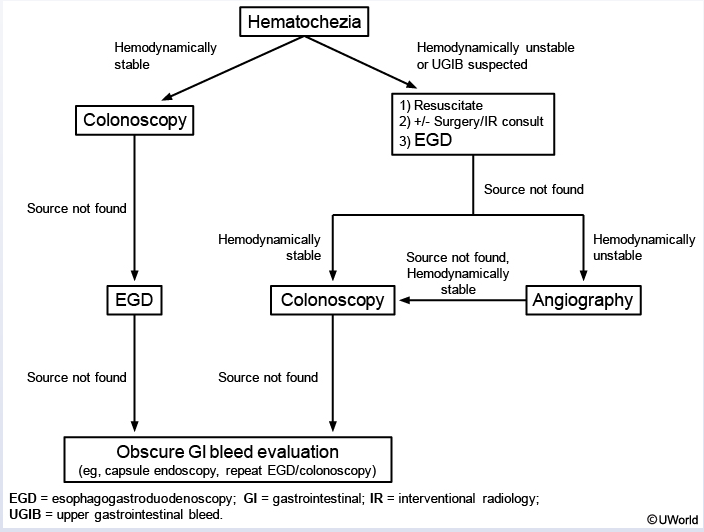
- This patient’s borderline-low blood pressure and tachycardia resolved with fluid resuscitation, and he has remained hemodynamically stable with no evidence of continued bleeding. No blood was aspirated on nasogastric lavage, and his BUN/Cr ratio is not elevated. He likely has LGIB rather than brisk UGIB therefore, bowel preparation (eg, laxatives) followed by colonoscopy is the first step to localize and potentially treat the source of hemorrhage. If no bleeding source is found, esophagogastroduodenoscopy (EGD) is performed. If EGD does not reveal a bleeding source, evaluation for obscure sources of GI bleeding should be considered (eg, video capsule endoscopy).
- In patients who are hemodynamically unstable or in whom UGIB is suspected, EGD should be considered first to exclude a brisk UGIB. Angiography or a nuclear medicine test (eg, tagged red blood cell) with radioactive tracer can be considered if a source cannot be identified on EGD; these require active bleed loss for visualization of the bleeding site.