hepatopulmonary syndrome
- related: GI gastroenterology, Pulmonary Diseases
- tags: #literature #pulmonology
Bubble echocardiography is typically diagnostic of hepatopulmonary syndrome (HPS), with infused microbubbles appearing on the heart’s left side after four to six cardiac cycles, contrasting this condition to an atrial septal defect that typically demonstrates left heart bubbles after the first or second cardiac cycle. Not all patients with HPS have significant cirrhosis or other typical features of end-stage liver disease. The clues in this patient are the mild ascites, suggesting liver disease, and finger clubbing, common in these types of shunts. Mortality in patients with cirrhosis is higher if they have HPS, independent of age, Model for End-Stage Liver Disease score, and hypoxemia, with an average survival of just 2 years without liver transplantation.
HPS is thought to arise from an imbalance of pulmonary vasodilators and vasoconstrictors in the setting of portal hypertension. Vasodilation and angiogenesis result in pulmonary capillaries enlarging from the usual diameter of 8 to 15 µm to 15 to 500 µm. This ventilation-perfusion mismatch may cause significant hypoxemia, and resting pulse oximetry <96% has been purported by some to be a threshold for HPS screening. These vascular abnormalities occur more distinctly in the lung bases, which can explain the supine improvement in oxygenation (orthodeoxia) and dyspnea (platypnea) of HPS. Patients often have skin telangiectasias and finger clubbing.
Oxygen supplementation is the mainstay of treatment, although it does not benefit all with HPS before or after liver transplantation. In patients undergoing liver transplantation, hypoxemia typically improves in 6 to 12 months (choice A is incorrect), but 15% to 20% fail to have significant improvement in hypoxemia. In contrast to portopulmonary hypertension, pulmonary artery pressure is not typically elevated, and the addition of vasodilator therapy may make this condition worse (choice B is incorrect). Typical pulmonary function tests are similar to those for patients with pulmonary hypertension in that spirometry and lung volumes may be normal, with isolated defects in diffusion. Pursuing complete pulmonary function tests when the patient has classic findings on bubble echocardiography is unlikely to add much to the diagnosis or management of this patient (choice C is incorrect). This patient’s history of rheumatoid arthritis may predispose him to pulmonary hypertension, but the relationship to HPS is likely coincidental.
Source
Hepatopulmonary syndrome is a complication of cirrhosis caused by dilation of the pulmonary vasculature in the setting of advanced liver disease and portal hypertension. A high alveolar-arterial oxygen gradient results from functional shunting. Patients with hepatopulmonary syndrome usually have a preexisting diagnosis of liver disease and present with shortness of breath. Dilation of pulmonary vasculature occurs at the base of the lungs, so hypoxemia is most noted when patients are upright or sitting, when shunting is maximal. Classic features are platypnea (worsening shortness of breath in the upright position) and orthodeoxia (worsening arterial oxygen saturation in the upright position). Pulse oximetry is often used to screen for changes in the arterial oxygen saturation level with changes of position. The diagnosis is made by demonstrating an arterial oxygen tension less than 80 mm Hg (10.7 kPa) breathing ambient air, or an alveolar-arterial gradient of 15 mm Hg (2 kPa) or greater, along with evidence of intrapulmonary shunting on echocardiography with agitated saline or macroaggregated albumin study. The detection of intrapulmonary shunting of blood is best confirmed by echocardiography with agitated saline (also known as a bubble study), during which bubbles are identified in the left side of the heart after 5 beats, demonstrating that the shunting of blood is not intracardiac. Clinically significant hepatopulmonary syndrome is treated with supplemental oxygen and liver transplantation. Hepatopulmonary syndrome is a progressive condition that is ultimately fatal without liver transplantation.
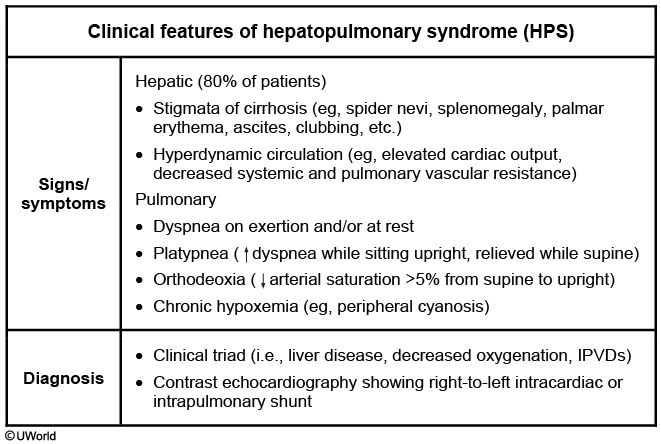
Hepatopulmonary syndrome is seen in 5%-40% of chronic liver disease patients. It is associated with portal hypertension, and usually presents years after the onset of chronic liver disease of any etiology. Patients typically present with the classic triad of liver disease, hypoxemia, and intrapulmonary vascular dilatations (IPVDs). IPVDs cause right-to-left shunting, which results in cyanosis and hypoxemia.
The IPVDs can be demonstrated by contrast enhanced echocardiography (best method), nuclear scanning (more expensive, less sensitive), or pulmonary angiography (invasive, seldom preferred). Contrast echocardiography (eg, with agitated saline; “bubble study”) confirms intrapulmonary right-to-left shunt if the microbubbles passing through the dilated pulmonary vessels cause left heart opacification 3-6 heart beats after right heart opacification. There is no effective medical therapy for HPS, and liver transplant is recommended for patients with severe hypoxemia.