hepatorenal syndrome HRS
- related: GI gastroenterology
- tags: #literature #note
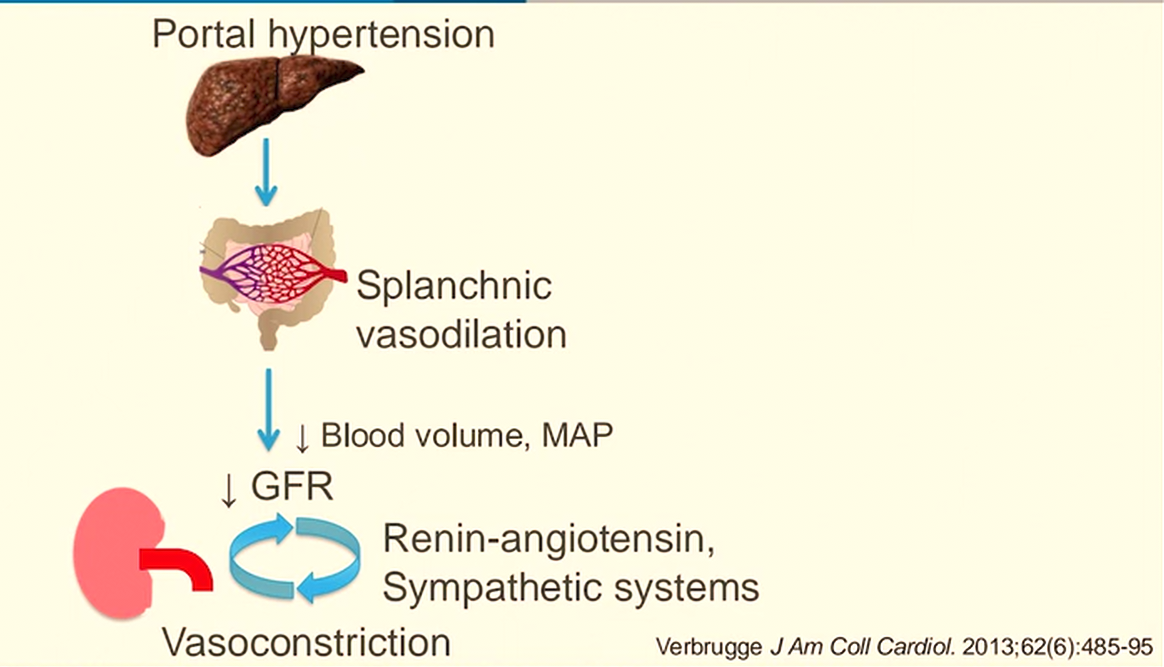
Pathophysiology
- important complication of end stage liver disease
- liver: cirrhosis => increased intrahepatic vascular resistance => portal HTN => increase NO, vasodilators => splanchnic arterial dilation (celiac, superior mesenteric, and inferior mesenteric arteries) => hypotension
- kidney: decrease in renal perfusion => activates RAAS/vasopressin => renal vasoconstriction with decreased perfusion and glomerular filtration.
Triggers:
- Decreased perfusion/volume:
- GI bleed, sepsis, vomiting, diuretic use, NSAID use
- ascites
- too much lactulose
- SBP
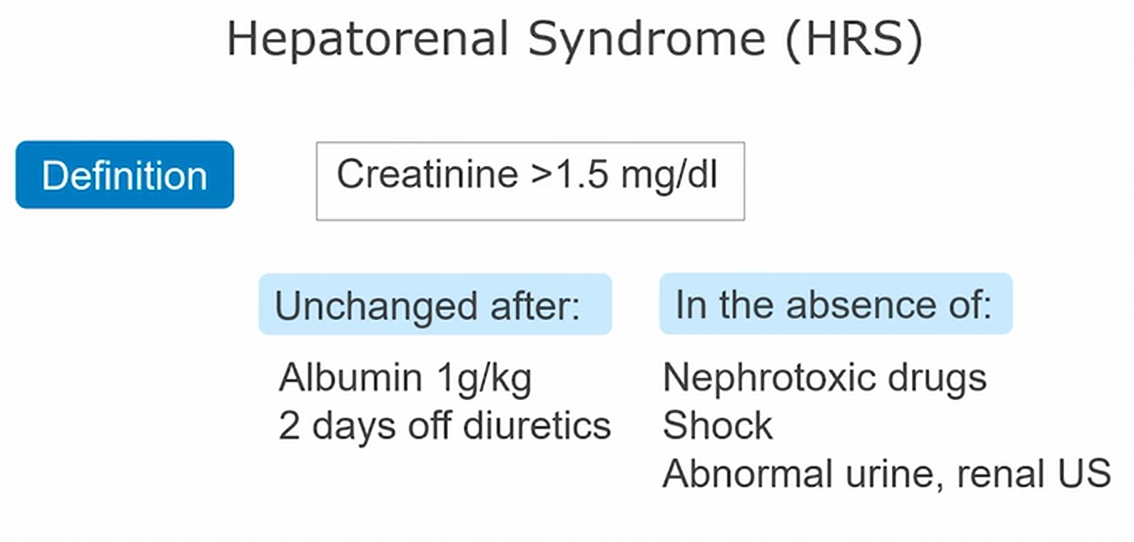
Diagnosis
- decreased renal perfusion (decrease in GFR) without another clear cause
- Cr > 1.5
- BUN:Cr elevated > 20:1
- no tubular injury: no RBC, protein, granular casts in urine
- protein excretion < 500 mg/d
- no microhematuria (<50 RBC per HPF)
- no obstruction: US benign
- Hyponatremia (dilutional hyponatremia)
- low Na excretion in urine (<10 mmol/L)
- lack of improvement with volume resuscitation (BUN:Cr could be high in either prerenal or hepatorenal)
- look for triggers: paracentesis if has ascites
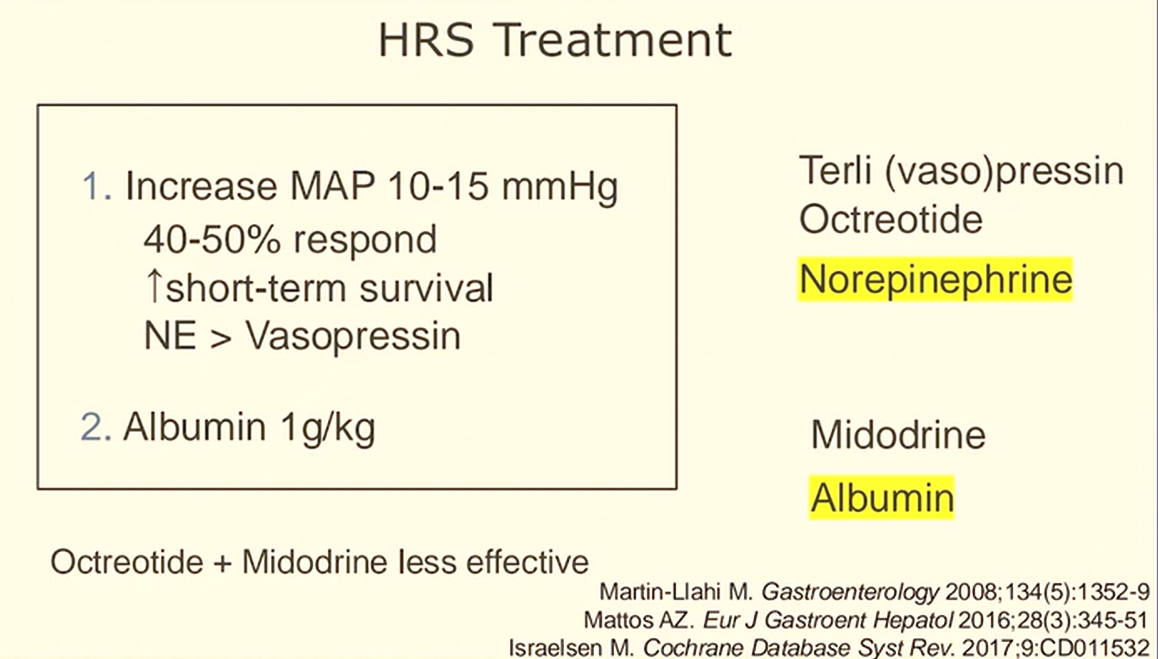
Treatment
- Goal: increase MAP > 82 (raise map by 10)
- Address triggers (hypovolemia, anemia, infection)
- Limit diuretics, beta blocker
- Plasma expander albumin
- IV bolus (1g/kg per day, up to 100g max) on 1st day
- followed by 25-50g/day until midodrine/octreotide discontinued
- continue 2-3 days
- Splanchnic vasoconstrictors
- midodrine (alpha agonist): 7.5 mg, titrate q8h up to 15 mg TID
- octreotide (inhibits vasodilation): gtt 50 mcg/hr or 100-200 mcg SQ q8h
- norepinephrine
- Increase urine output to at least 200 cc/4 hours
- TIPS
- discontinue therapy if no response after 4 days
- dialysis/transplant is next option
- Liver transplant
- Dialysis may be attempted to help bridge to liver transplantation.
Complications
- Cr greater AND off steroids for 2 days AND have tried albumin
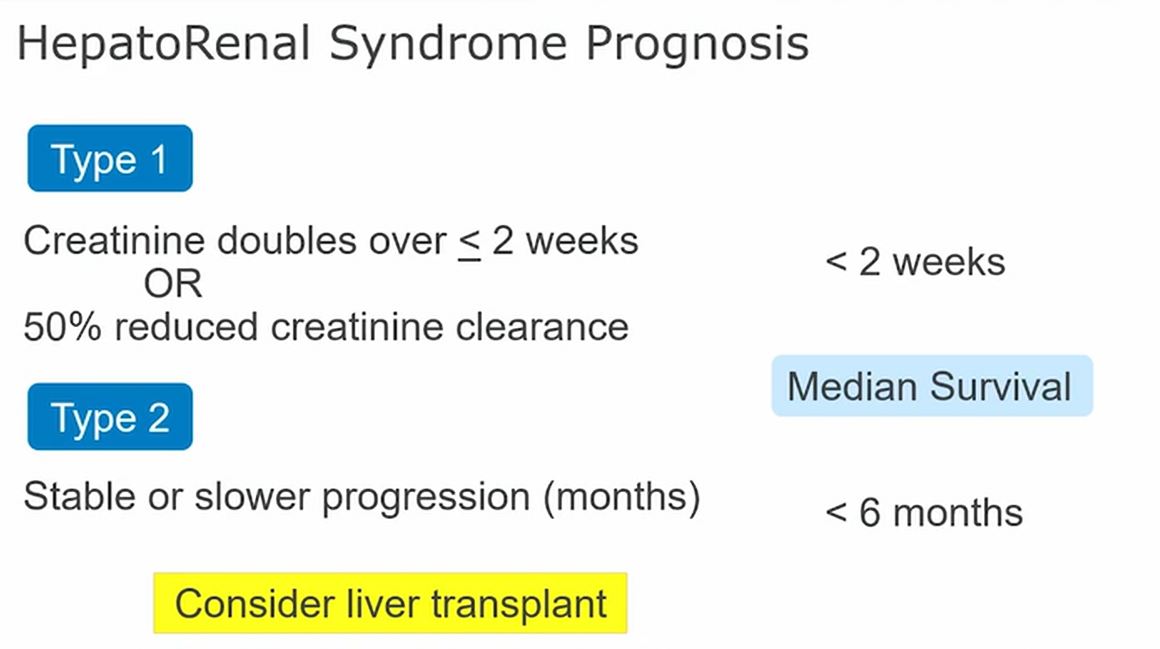
- type 1 progresses rapidly
- prerenal state
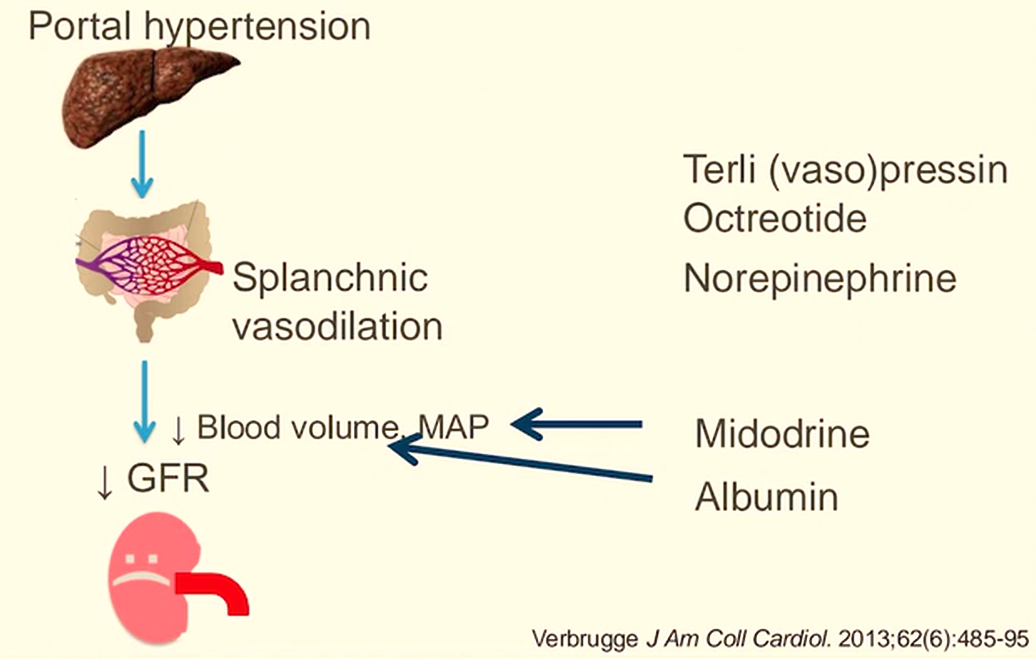
- terlipressin or vasopressin
- In ICU, data is for pressor and albumin
- levo early1
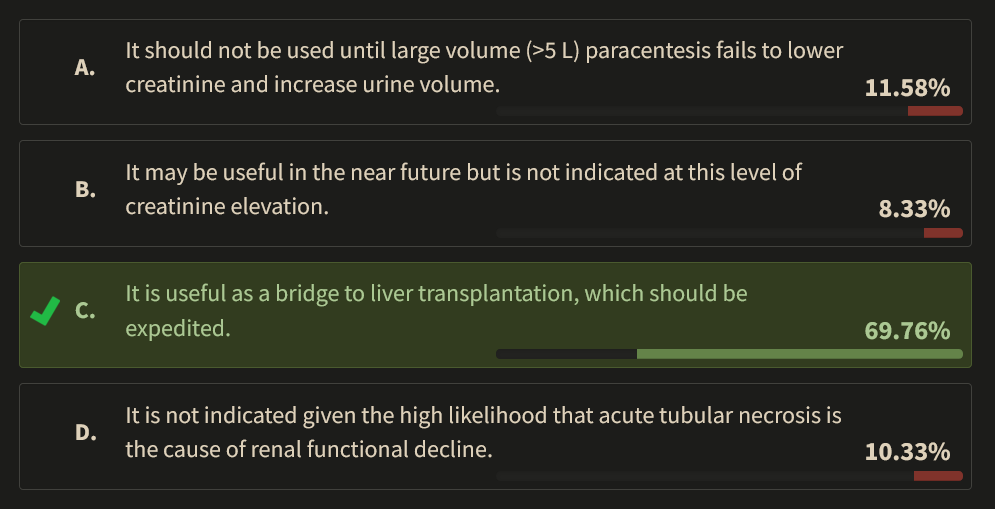
AKI is a common condition in patients with cirrhosis, with estimates of an incidence of 50% in hospitalized patients with cirrhosis and higher in patients with cirrhosis admitted to the ICU. As for all cases of AKI, the clinician must consider prerenal, intrinsic renal, and postrenal causes. Patients with cirrhosis may exhibit an additional pathology, HRS, which is thought to arise from the vascular effects of portal hypertension and increased abdominal pressure, with a redirection of blood flow away from the kidneys despite replete circulation. Thus, the patient with HRS may not exhibit the findings of hypovolemia on examination or by ultrasound assessment yet will show measurements of low fractional excretion of sodium and urea typical of hypovolemia that are relied upon by clinicians to distinguish between prerenal causes of AKI and intrinsic renal injury such as acute tubular necrosis (ATN). In studies of patients hospitalized with AKI complicating cirrhosis, approximately half had AKI ascribed to hypovolemia, 30% to ATN, and 15% to 20% to HRS. Postrenal obstruction was rarely found to be a cause of AKI in these patients. In the patient presented here, the findings on urinalysis and excretion parameters effectively exclude ATN (choice D is incorrect).
In the past, HRS was divided into types 1 and 2; in the former, the evolution of kidney injury was over 2 weeks or less, and in the latter, the injury evolved over longer time frames. Over the past decade, these definitions have been replaced with thresholds and terminology more in harmony with recommendations of the Kidney Disease: Improving Global Outcomes (KDIGO) initiatives. HRS-AKI, the new term, is defined as an increase in the serum creatinine level of 0.3 mg/dL (26.52 µmol/L) within 48 h or an increase in the serum creatinine that is at least 1.5 times the baseline level over the past 7 days. These definitions are meant to provide criteria for early identification and treatment of patients (choice B is incorrect). Slower deterioration of renal function consistent with HRS is now termed HRS with chronic kidney disease.
Since morbidity and mortality are high for patients with nonresolving HRS-AKI, identification of therapies to treat or prevent this complication of cirrhosis is an important priority. There is no strong evidence that large-volume paracentesis improves outcomes in patients with HRS-AKI, despite the theoretical benefits of reducing intraabdominal pressure, and this procedure risks inducing hypovolemia and compounding renal injury (choice A is incorrect). Thus, large-volume paracentesis should be reserved for symptom control in patients with tense ascites, and volume removal should be accompanied by albumin infusion. On the basis of several series and a randomized trial, both United States and European guidelines recommend terlipressin as a first-line treatment for HRS-AKI. The primary adverse effect of terlipressin administration is the development of respiratory failure due to pulmonary edema, and it should not be given to patients with severe hypoxemia, vascular congestion or pulmonary edema by imaging, or obvious volume overload apart from expected ascites and peripheral edema. Patients should be monitored closely for the development of pulmonary edema during terlipressin infusion. Norepinephrine has also been used to enhance renal function in patients with cirrhosis who have HRS-AKI but is less studied for this indication, was infused during this patient’s decline in renal function, and was not offered as an answer choice. Terlipressin has not been shown to enhance survival in patients with HRS-AKI but is an effective bridge to liver transplantation, which when successful can fully correct HRS.23456
A 55-year-old with long-standing and progressive alcoholic cirrhosis is hospitalized for sepsis secondary to spontaneous bacterial peritonitis. The patient has been abstinent from alcohol for 1 year and was listed for transplantation 2 months ago, with an estimated wait time of 3 to 6 months.
Four days ago, the patient presented to the liver clinic with fever and moderate abdominal pain. Paracentesis revealed WBC count of 650 polymorphonuclear leukocytes per cubic millimeter. Broad-spectrum antibiotics were begun, and 1.5 g albumin/kg was given intravenously initially and repeated on day 3. In view of slightly diminished BP, necessitating low-dose norepinephrine infusion, the patient was admitted to the ICU.
From an infection perspective, the patient has done well, with resolution of fevers, abdominal pain, leukocytosis, and hypotension. Norepinephrine has been discontinued. Peritoneal cultures recovered a pan-sensitive Escherichia coli. However, over the course of the ICU stay, renal function has declined. Despite positive fluid balance of 0.5 to 1 L/day, urine output has declined to an oliguric range. The patient’s creatinine level has risen from a baseline level of 0.7 to 1.6 mg/dL (61.88 to 141.44 µmol/L). Evaluation has included renal ultrasound (normal-sized kidneys with no evidence of obstruction), urinalysis (no casts, RBCs, or WBCs), and measurement of fractional excretion of sodium (<0.1%) and urea (<20%). Examination reveals 1+ pitting edema of the lower extremities and prominent ascites with a fluid wave. The jugular venous waveform is visible, estimating a right atrial pressure of 10 mm Hg. The patient has a clear chest radiograph and SpO2 of 97% while breathing ambient air. Point-of-care ultrasound cannot visualize the inferior vena cava well because of the hyperechoic liver, but cardiac evaluation does not suggest ventricular underfilling.
Which of the following is true about terlipressin use in this setting?
Links to this note
-
most common complication of HRS treatment includes respiratory failure
- related: hepatorenal syndrome HRS
Footnotes
-
Amathieu R, Al-Khafaji A, Sileanu FE, et al. Significance of oliguria in critically ill patients with chronic liver disease. Hepatology. 2017;66(5):1592-1600. PubMed ↩
-
Nadim MK, Garcia-Tsao G. Acute kidney injury in patients with cirrhosis. N Engl J Med. 2023;388(8):733-745. PubMed ↩
-
Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999;341(6):403-409. PubMed ↩
-
Wong F, Pappas SC, Curry MP, et al; CONFIRM Study Investigators. Terlipressin plus albumin for the treatment of type 1 hepatorenal syndrome. N Engl J Med. 2021;384(9):818-828. PubMed ↩