how to clear cervical collar
- related: ICU intensive care unit
- tags: #literature #icu
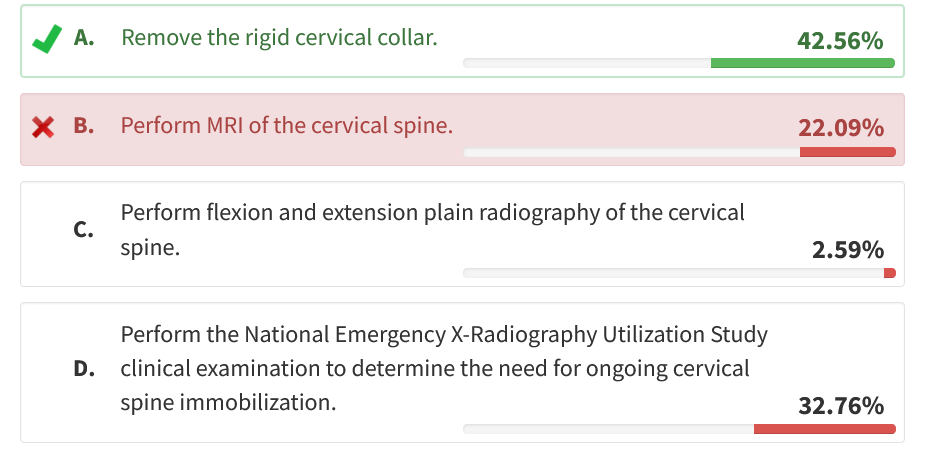
Therefore, the appropriate next step is to attempt to clear his cervical spine clinically and remove the collar.
Clinical clearance of the cervical spine is predicated on three conditions: (1) the mechanism of injury is not one with a high risk of developing cervical spine injury, (2) the patient was not intoxicated or impaired at the time of the injury, and (3) the patient can cooperate with the examination and report pain.
Low risk injury is defined as the absence of a high-speed motor vehicle crash at more than 35 mph (>56 kph), death of another person involved in the same motor vehicle crash, fall from more than 10 ft (>3 m), significant closed head injury or hemorrhage at head CT scanning, neurologic symptoms or signs referred to the cervical spine, or pelvic or multiple extremity fractures.
In patients who have a low-risk mechanism of injury, a normal spine CT scan, and the ability to cooperate with the examination, clinical clearance is appropriate. The evaluation consists of removing the anterior part of the collar and asking the patient to flex and extend the neck and rotate the head from side to side without resistance. If there is no restriction of movement or pain, the motions are repeated against mild resistance (with a hand). If there is no pain to resistance, the neck can be considered cleared and the collar removed.
In patients with a low risk of cervical injury who cannot have a cervical spinal injury ruled out by using a clinical decision tool such as the National Emergency X-Radiography Utilization Study (NEXUS) criteria, the Eastern Association for the Surgery of Trauma recommends multidetector CT scanning of the cervical spine as the primary method of screening (which was already performed in this patient). This imaging test has a negative predictive value of more than 99%, including in patients with intoxication and those who are obtunded. Given that this patient has a low risk of cervical spine injury and a normal CT scan of the cervical spine, it is reasonable for the ICU physician to remove the rigid cervical collar and, perhaps, avoid complications of rigid cervical collar use such as new pressure injuries of the neck.
In patients in whom the clinical clearance fails and in those who are not able to cooperate with the examination or who have a more severe mechanism (such as a fall from height or a severe motor vehicle crash), there is controversy over the appropriate management. Three options have been entertained. The most conservative option is to leave the patient in a collar for 6 weeks and reevaluate. This was thought to be the safest option, but recognition that skin breakdown around the collar is a serious complication has called this into question. The second option is to perform MRI of the cervical spine to investigate ligamentous injury that could make the spine unstable without bony injury. Clearance based on MRI testing has not been evaluated rigorously but is practiced extensively. The final option is to clear the spine with only CT scanning evidence. Because the risk of ligamentous injury is low if there are no findings of soft-tissue swelling on CT scans, this option is defensible but relies on a degree of comfort with the uncertainty that a small proportion of patients with unstable spines may be missed. This third option is gaining acceptance in medical cultures around the world.1234567
A 42-year-old man with alcohol use disorder presented after bystanders witnessed him stumble and then fall to the ground while bracing himself with outstretched arms. Emergency medical services placed him in a rigid cervical collar, administered intramuscular midazolam for agitation, and transported the patient to the emergency department.
In the emergency department, he was awake but with severe agitated delirium. Although he was not following commands or answering questions, he was using both arms purposefully to grab objects and was able to stand on his own and walk during an episode of agitation. He had no other injuries detected at physical examination. He was then admitted to the ICU after initiation of a continuous infusion of dexmedetomidine for agitated delirium. His blood ethanol level was 432 mg/dL (93.79 mmol/L; normal, <50 mg/dL [<10.85 mmol/L]). CT scanning without contrast material of the head and neck revealed no acute injury.
Which of the following is the best next step in the management of the patient’s possible cervical injury?
Links to this note
Footnotes
-
Moeri M, Rothenfluh DA, Laux CJ, et al. Cervical spine clearance after blunt trauma: current state of the art. EFORT Open Rev. 2020;5(4):253-259. PubMed ↩
-
Bush L, Brookshire R, Roche B, et al. Evaluation of cervical spine clearance by computed tomographic scan alone in intoxicated patients with blunt trauma. JAMA Surg. 2016;151(9):807-813. PubMed ↩
-
Como JJ, Diaz JJ, Dunham CM, et al. Practice management guidelines for identification of cervical spine injuries following trauma: update from the eastern association for the surgery of trauma practice management guidelines committee. J Trauma. 2009;67(3):651-659. PubMed ↩
-
Hasandarras AKH, Strandvik GF, Faramawy AE, et al. Intensive care physician-led clearance of the cervical spine: a retrospective review of the utility of a normal cervical CT scan for safe removal of hard collars by critical care physicians. J Intensive Care Med. 2023;38(10):903-910. PubMed ↩
-
Inaba K, Byerly S, Bush LD, et al; WTA C-Spine Study Group. Cervical spinal clearance: a prospective Western Trauma Association Multi-institutional Trial. J Trauma Acute Care Surg. 2016;81(6):1122-1130. PubMed ↩
-
Patel MB, Humble SS, Cullinane DC, et al. Cervical spine collar clearance in the obtunded adult blunt trauma patient: a systematic review and practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015;78(2):430-441. PubMed ↩