ILD associated with MDA-5 dermatomyositis
- related: ILD Interstitial Lung Disease or Diffuse Parenchymal Lung Disease
- tags: #literature #pulmonology
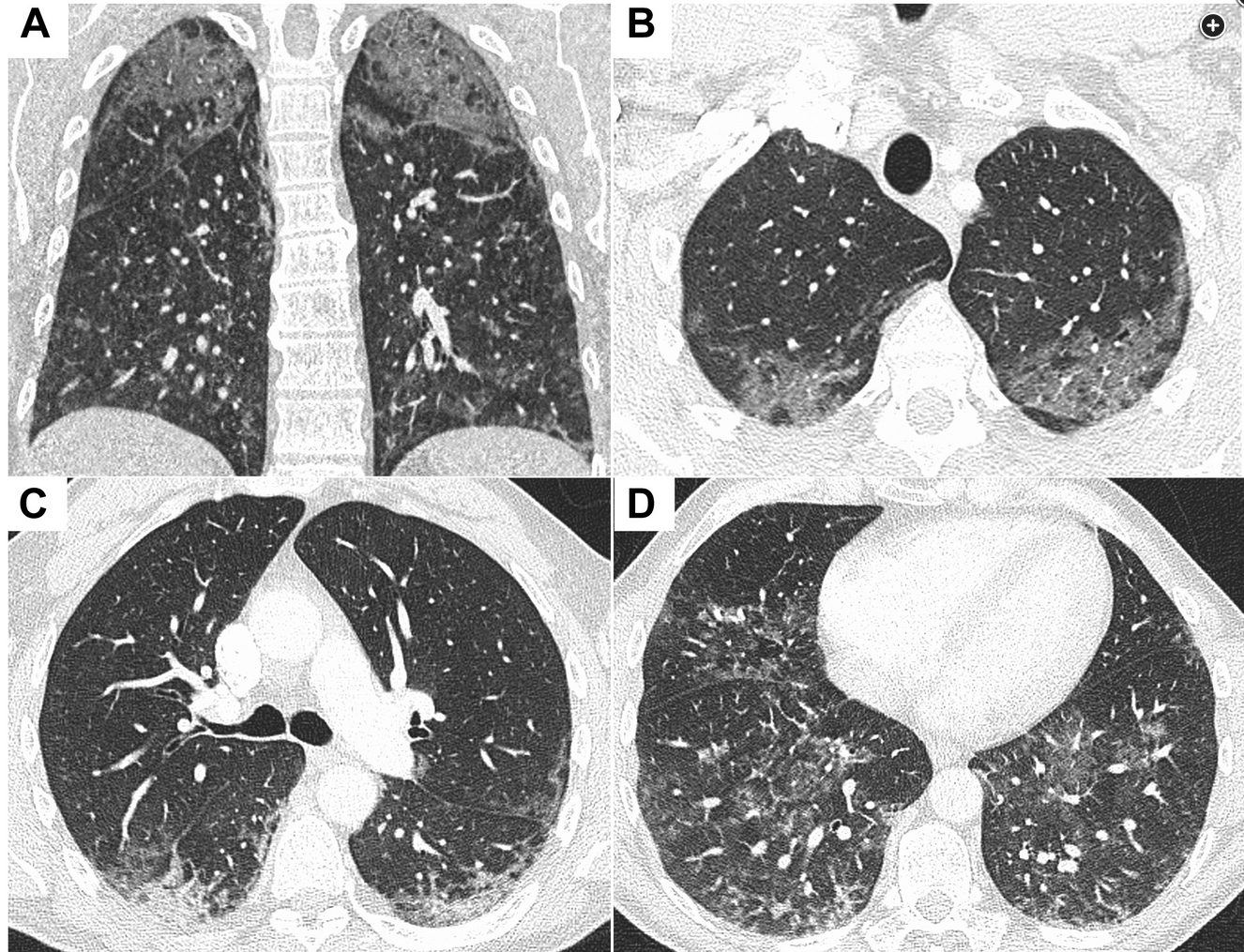
- sx: fever, rapidly progressive pulmonary disease, hyperkeratosis/periungual erythema
- labs: anti-MDA-5 antibody
- important: little to no myositis in comparison to other myositis associated lung disease
Dermatomyositis is a heterogeneous disease with many subtypes that are differentiated by symptoms, clinical course, and myositis-specific antibodies. This patient experienced a rapidly progressive pulmonary disease with fever and minimal evidence of myopathy. His skin findings reveal hyperkeratosis and periungual erythema with dilated nail fold capillaries. This combination of findings is most consistent with interstitial lung disease associated with anti-melanoma differentiation-associated protein-5 (MDA-5) dermatomyositis. The anti-MDA-5 antibody was first identified nearly 20 years ago among a cohort of patients with dermatomyositis who had little to no myositis and was associated with rapidly progressive interstitial lung disease in nearly all patients. The antibody targets the MDA-5 protein, which is involved with the innate immune system and recognizes double-stranded RNA viruses inducing a type 1 interferon response on recognition. The anti-MDA-5 antibody is specific to dermatomyositis and helps differentiate it from other inflammatory lung diseases. There may be environmental factors and/or genetic predisposition explaining the varying prevalence of anti-MDA-5 among dermatomyositis patients in Japan (20%-40%) and Europe (7%-10%).
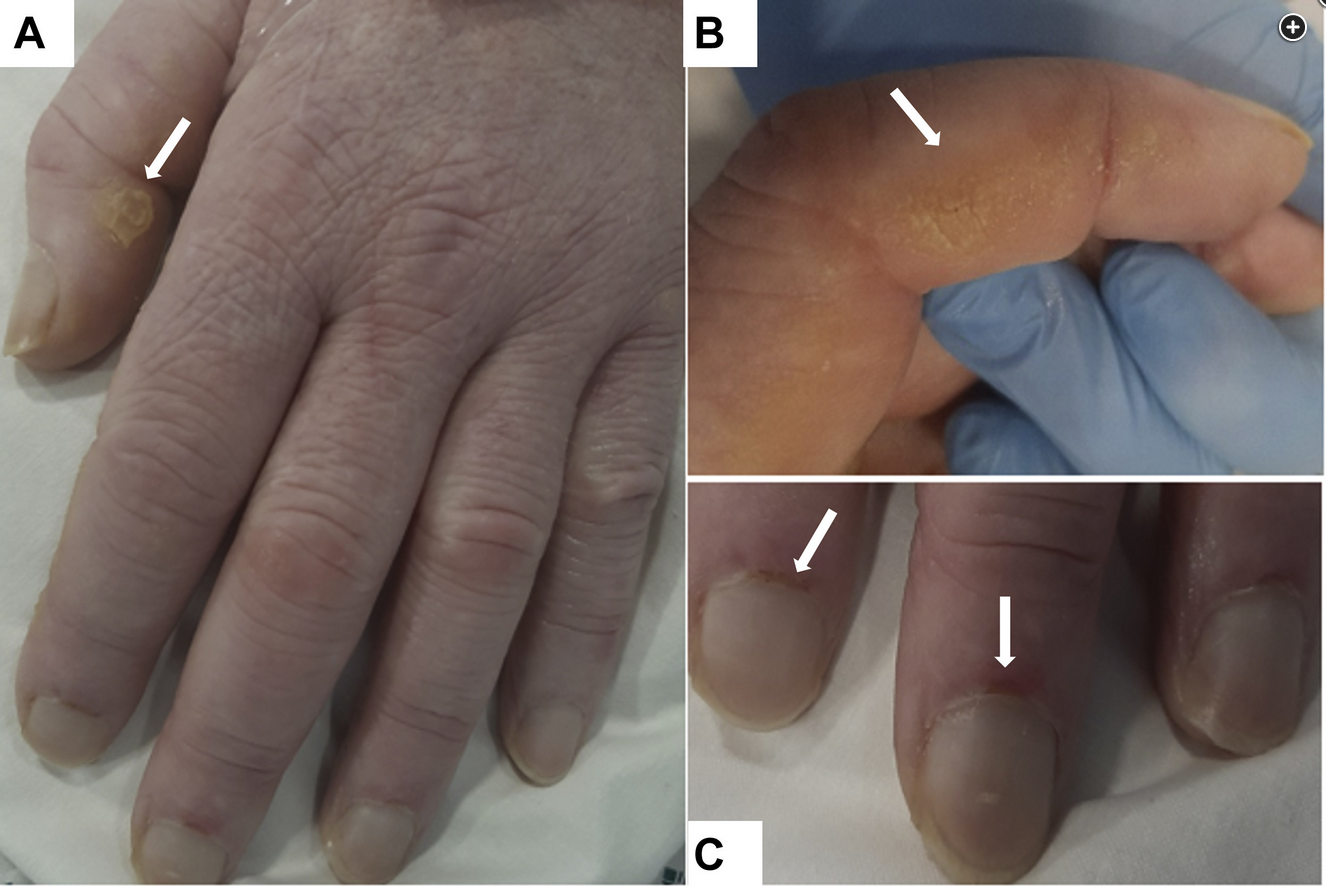
- Photographs showing hyperkeratosis and skin cracking (A and B) and periungual erythema and dilated nail fold capillaries (C).
Anti-Jo-1, anti-EJ, and anti-PL-7 are all more common in the antisynthetase syndrome in which clinical features can also include fevers, arthralgias, and mechanic’s hands, but they are more typical for myositis (50%-90%) and symptoms of proximal muscle weakness, both of which were absent in this patient. The clinical course in patients with antisynthetase syndrome is usually more chronic or subacute, unlike this patient’s rapid deterioration.
From a clinical standpoint, early recognition and treatment of this anti-MDA-5 subtype of dermatomyositis can result in a significant improvement in outcomes. When compared with corticosteroid therapy alone, combination immunosuppressant therapy of corticosteroids plus other agents (eg, IV cyclophosphamide, tacrolimus, rituximab) and immunoglobulins have shown better 6-month survival (89% vs 33%) when started early. Plasma exchange has also been used with some success.1