initiating nighttime NIV for chronic hypercapnia in COPD
- related: Sleep and Sleep Disordered Breathing
- tags: #literature #pulmonology
- consider initiating once awake PCO2 > 52 mmHg
- European guideline and ATS have different recommendation for acute hospitalized patients:
- European guideline favors starting NIV after acute COPD exacerbation in hospital
- ATS recommend waiting 2-4 weeks after discharge with reassessment outpatient
Current recommendations suggest initiating long-term nocturnal noninvasive ventilation (NIV), in addition to optimized usual care, for patients with chronic stable hypercapnic COPD 2 to 4 weeks following discharge from hospital for an acute exacerbation of COPD (AECOPD). It is further suggested that, if appropriate, patients with chronic stable hypercapnic COPD undergo screening for OSA before consideration of long-term NIV.
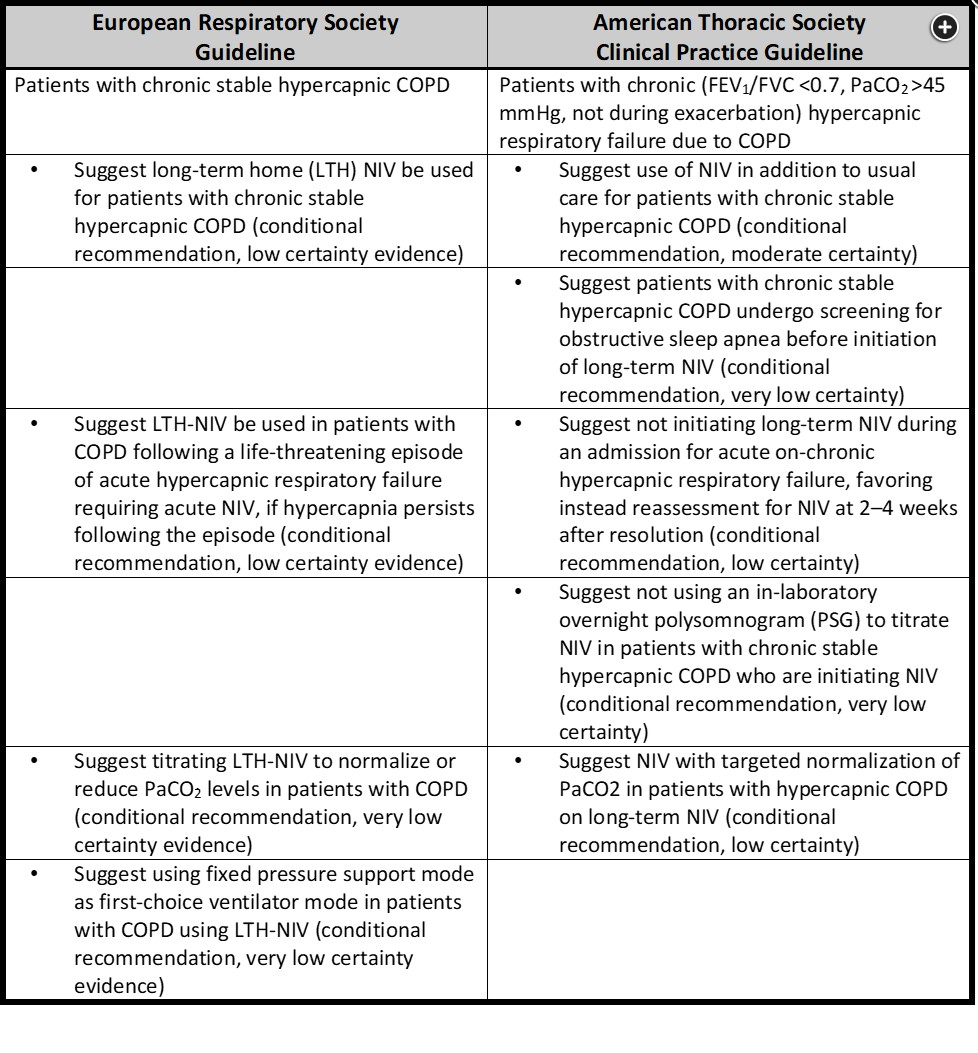
Acute NIV is well established to improve important outcomes significantly in patients with COPD and acute life-threatening hypercapnic respiratory failure. It is also well known that patients admitted to hospital for AECOPD requiring acute NIV, and with persistent hypoxemia and hypercarbia following stabilization, have a very poor prognosis following discharge, with median time to readmission or death significantly less than a year. The evidence for benefit of long-term NIV in stable COPD in this setting is less certain, although recent research findings have demonstrated that, among patients with persistent hypercapnia following AECOPD, adding long-term NIV to home O2 supplementation significantly improves the composite index of time to readmission or death within 12 months. Following systematic review and assessment of all published literature to date, clinical practical guidelines published in 2019 and 2020 suggest long-term nocturnal NIV for chronic stable hypercapnic COPD because of reductions in hospitalization and mortality, as well as improvements in awake gas exchange, functional activity, 6-min walk distance, dyspnea, and quality of life. While limitations in the published literature were noted, there was overall consistency of the direction of effect in favor of improvement with NIV therapy in this setting. A summary and comparison of recommendations and evidence from the European Respiratory Society and American Thoracic Society clinical practice guidelines are provided in Figure 1. It is recognized that these recommendations may change with further research in the future. Therefore, areas for future investigation were highlighted, and barriers to widespread implementation, including cost, were recognized and identified. It was particularly emphasized that if long-term nocturnal NIV was implemented, it should be purposefully goal-directed toward normalization or reduction of the PaCO2 and overseen by experienced practitioners who routinely care for chronic hypercapnic COPD patients.1
This patient has severe COPD with stable hypercapnia. He has minimal risk factors for OSA (no snoring, witnessed apneas, or hypersomnolence; low BMI; and normal oropharyngeal examination). In these patients, initiating outpatient NIV with high-intensity ventilatory support during sleep has been shown to improve outcomes such as rehospitalization or mortality. Importantly, clinical trials that have shown beneficial effect of high-intensity NIV have been performed in patients who were ambulatory and had persistent hypercapnia (PaCO2 ≥52 mm Hg) a few weeks after hospital discharge. In randomized clinical trials, NIV settings were titrated to achieve at least 20% reduction in PCO2. This led to typical expiratory PAP (EPAP) of 4 to 5 cm H2O and inspiratory PAP (IPAP) of 22 to 26 cm H2O and backup respiratory rate of 14 to 16/min, leading to high levels of pressure support (ie, high-intensity NIV).