intracranial pressure ICP and cerebral perfusion pressure goals and treatment in TBI
- related: traumatic brain injury overview
- tags: #literature #icu
The goal in traumatic brain injury is to keep cerebral perfusion pressure, or CPP, above 60 mmHg. CPP is the pressure necessary to maintain cerebral blood flow. It’s .
The two ways to improve CPP is to either improve MAP or decrease ICP. Blood pressure should be monitored:
- Keep SBP > 110 for patients <50 and >70
- Keep SBP > 100 for patients 50 - 60
- Permissive hypertension with SBP <180
- Use pressors with caution as they may increase ICP while increase the MAP. This happens more often in patients who have lost their autoregulation. In a normal person, increase in SBP only transiently increases ICP
The goal for ICP is less than 22. Treatment is often initiated for patients with ICP greater than 22. treatment for elevated ICP includes hypertonic saline and mannitol is discussed separately.
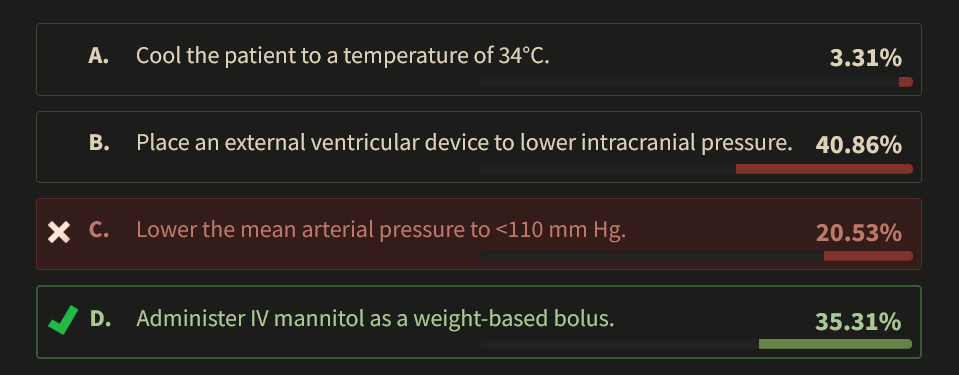
There are very few recommendations about the management of traumatic brain injury (TBI) that have been tested in randomized controlled trials. Therefore, management of intracranial pressure (ICP) in patients with TBI is based largely on retrospective associations and expert opinion. ICP values >20 mm Hg have consistently shown worse outcome (usually measured with the Glasgow Outcome Scale-Extended [GOSE]) in severe TBI and should be avoided. The GOSE is an 8-point scale that goes from 1 (dead) to 7 or 8, denoting return to normal life activities. In addition to ICP, inadequate BP to overcome the increased ICP has been associated with poor outcome. The calculated value for perfusion to the brain is called the cerebral perfusion pressure (CPP), which is calculated as mean arterial pressure (MAP) minus ICP (when the ICP is greater than central venous pressure). Until recently, the only recommendations about CPP were based on ensuring the lower value to ensure brain perfusion. Although there has been refinement of what is the appropriate lower value of CPP from 70 to 60 mm Hg, the more interesting guideline recommendation centered around the upper limit. In patients with focal lesions, a strategy to increase CPP >70 mm Hg using vasopressors and fluids is associated with worse neurological outcome on GOSE at 6 months. Although mechanistic work has suggested that patients with impaired autoregulation develop hyperemia and cerebral edema with elevated CPP values, lowering CPP to below 70 mm Hg in patients who achieve these values without augmentation has not been tested and may have consequences in peri-contusion ischemic tissue. The Traumatic Brain Injury Guidelines suggest “avoiding aggressive attempts to maintain CPP above 70 mm Hg with fluids and pressors may be considered because of the risk of adult respiratory failure”.
An external ventricular drain (EVD) is the preferred method of lowering ICP in patients with traumatic brain injury when it can be achieved safely. In this patient, the frontal horns of the lateral ventricles are compressed; EVD placement carries a high risk of failure and injury.
Lowering body temperature as a primary method of improving outcome in TBI was tested in the POLAR trial and failed to show benefit.12345
A 27-year-old man with a history of two previous motor vehicle crashes due to ethyl alcohol intoxication is an unrestrained driver in a single-vehicle collision with a road barrier that ejected him from the car. In the field, he is unconscious with a Glasgow Coma Scale score of 4 and undergoes intubation. In the ED, a CT scan of the head shows a large right frontal contusion and anterior temporal contusions in both hemispheres. The frontal horns of his lateral ventricle are compressed. Because of his low Glasgow Coma Scale score and focal lesions, he has an intracranial pressure monitor placed for management of increased intracranial pressure. His intracranial pressure on placement is 40 mm Hg. His heart rate is 90/min, and his BP is 180/80 mm Hg (mean arterial pressure, 113 mm Hg).
What is the best intervention to improve the patient’s outcome?
Links to this note
-
treatment for elevated ICP includes hypertonic saline and mannitol
-
related: intracranial pressure ICP and cerebral perfusion pressure goals and treatment in TBI, traumatic brain injury overview
-
Give hypertonic saline for patients with elevated ICP (intracranial pressure ICP and cerebral perfusion pressure goals and treatment in TBI)
-
Footnotes
-
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery. 2017;80(1):6-15. PubMed ↩
-
Cooper DJ, Nichol AD, Bailey M, et al; POLAR Trial Investigators and the ANZICS Clinical Trials Group. Effect of early sustained prophylactic hypothermia on neurologic outcomes among patients with severe traumatic brain injury: the POLAR randomized clinical trial. JAMA. 2018;320(21):2211-2220. PubMed ↩
-
Lowering body temperature as a primary method of improving outcome in TBI was tested in the POLAR trial and failed to show benefit.123 ↩
-
Robertson CS, Valadka AB, Hannay HJ, et al. Prevention of secondary ischemic insults after severe head injury. Crit Care Med. 1999;27(10):2086-2095. PubMed ↩