Jarisch-Herxheimer reaction from borreliosis treatment
- related: Infectious Disease ID
- tags: #literature #id
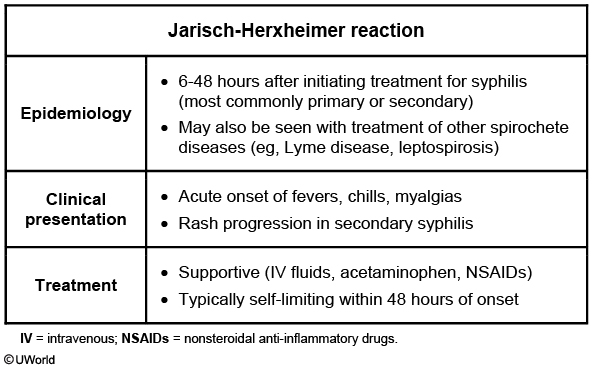
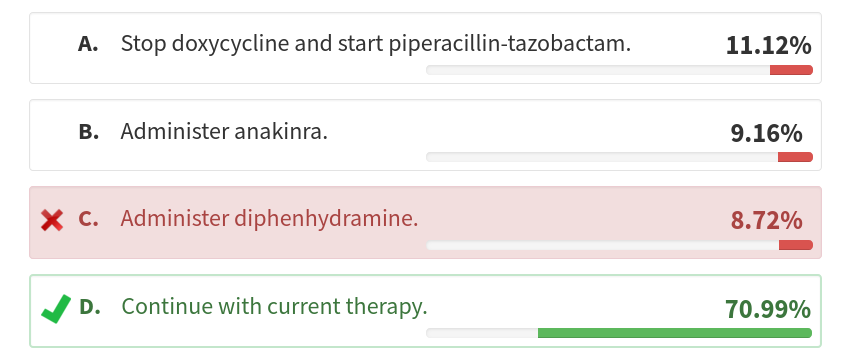
The patient has a history and presentation consistent with a Jarisch-Herxheimer reaction complicating antibiotic therapy for borreliosis, in this case most likely tick-borne relapsing fever. Although Jarisch-Herxheimer reactions are classically associated with antibiotic therapy for syphilis, they may be associated with other spirochetal diseases, including borreliosis and leptospirosis. Although doxycycline is the typical antibiotic treatment for borreliosis, β-lactams are also effective and commonly trigger a Jarisch-Herxheimer reaction in a patient with tick-borne relapsing fever. The pathophysiology of the Jarisch-Herxheimer reaction is thought to be the rapid killing of a high titer of spirochetes, which are more immunogenic after cell death than before. Although Jarisch-Herxheimer reactions can be severe, they generally resolve quickly with usual supportive care (eg, IV fluids, as in this case) and should not result in change in antibiotic therapy, as they are an indication that the therapy is effective (choice D is correct; choice A is incorrect).
Hypotension after antibiotic therapy may indicate anaphylaxis, which is an important consideration in patients presenting with a Jarisch-Herxheimer reaction. Anaphylaxis can cause tachycardia and hypotension, and abdominal symptoms of anaphylaxis can be mistaken for the truncal pain (a manifestation of elevated cytokine levels) of a Jarisch-Herxheimer reaction. However, the presence of a tick bite, the absence of drug allergies, and the rigors with hypertension are all more consistent with a Jarisch-Herxheimer reaction, so antihistamines are not indicated (choice C is incorrect).
The other major consideration in a patient with possible Jarisch-Herxheimer is progressive sepsis. In this case, results of urinalysis, chest radiography, echocardiography, and CBC count are normal, and the pattern of recurring fevers after a tick bite while exploring caves in Utah with dramatic cytokine release after administration of a β-lactam antibiotic makes Jarisch-Herxheimer reaction more likely than sepsis, so broadening of antimicrobials is not indicated (choice A is incorrect).
Whether to treat (or, more often, prevent) Jarisch-Herxheimer reactions in patients with spirochetal infections through use of immunomodulators is somewhat controversial. Older data suggest that antibodies against tumor necrosis factor α and/or glucocorticoids may prevent or attenuate a Jarisch-Herxheimer reaction. This has not been well investigated in borreliosis, but in severe cases, glucocorticoid therapy may be reasonable, although the generally benign course of Jarisch-Herxheimer reactions with supportive care argues against routine use of glucocorticoids. In any case, use of anakinra (an IL-1 antagonist approved to treat rheumatoid arthritis and increasingly used off-label to treat hemophagocytic lymphohistiocytosis) is well beyond any available evidence and would not be an appropriate treatment for this patient (choice B is incorrect).
The various relapsing fevers are caused by Borrelia species, some carried by lice, some by ticks. In North America, the most common causes are Borrelia hermsii, Borrelia turicatae, or Borrelia parkeri, which are spread via Ornithodoros tick bites. (Jarisch-Herxheimer reactions are less commonly observed in Borrelia burgdorferi infections—“Lyme disease”—but do occur.) As opposed to other zoonosis-carrying ticks, the causative ticks for tick-borne relapsing fever move directly from structures to humans. Thus, cave or cabin exposures (or camping among rodent nests) are considered typical exposures. In this case, the cave exposure in Utah would be most consistent with B hermsii infection. Often, tick bites are not recognized as such at the time but may be described as a small pimple.
A 30-year-old man presented to the emergency department with 4 days of fever, right upper quadrant discomfort, and cough. He returned 2 weeks ago from a camping trip in Utah, during which he and his friends explored caves. He was bitten by a tick on the back of his neck during the trip.
At presentation, his vital signs were a temperature of 38.2 °C, heart rate of 101/min, respiratory rate of 16/min, and BP of 120/55 mm Hg. Results of urinalysis, a CBC count, and a comprehensive metabolic panel were normal. Results of right upper quadrant ultrasonography and chest radiography were normal. After confirmation that the patient has no drug allergies, doxycycline was started while further diagnostic testing was sent.
Four hours later, the patient experiences rigors and diffuse truncal pain. His vital signs are now a temperature of 39.2 °C, heart rate of 128/min, respiratory rate of 25/min, and BP of 160/100 mm Hg. The patient reports no pruritus, rash, abdominal pain, and tongue or throat swelling. Examination shows no evidence of urticaria and no throat, mouth, or tongue swelling. After 45 min, his BP drops to 90/55 mm Hg; examination results are otherwise unchanged. Bedside cardiac ultrasonography shows hyperdynamic left ventricular function, normal right ventricular size and function, and normal valve structure and function.
In addition to IV volume expansion, which of the following is the best next step in management?
Links to this note
Footnotes
-
Campbell SB, Klioueva A, Taylor J, et al. Evaluating the risk of tick-borne relapsing fever among occupational cavers-Austin, TX, 2017. Zoonoses Public Health. 2019;66(6):579-586. PubMed ↩
-
Dhakal A, Sbar E. Jarisch-Herxheimer reaction. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. PubMed ↩
-
Snowden J, Yarrarapu SNS, Oliver TI. Relapsing fever. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. PubMed ↩