leaks on a ventilator
- related: basic modes of ventilators
- tags: #literature #pulmonology #icu
The important change on the ventilator graphics is in the volume tracing where the inspiratory volume is markedly larger than the expiratory volume (Figure 2, arrow indicates when expiration is complete and the ventilator resets the volume to zero as it transitions into inspiration). This is a typical pattern in a circuit leak resulting from such things as a partial circuit disconnect, ruptured endotracheal tube cuff, or a large bronchopleural fistula. Under the right conditions (as in this case), a significant leak can overwhelm the ventilator’s leak compensation mechanisms, causing an airway pressure drop that the ventilator interprets as a patient effort and responds with delivery of repeated assisted breaths.
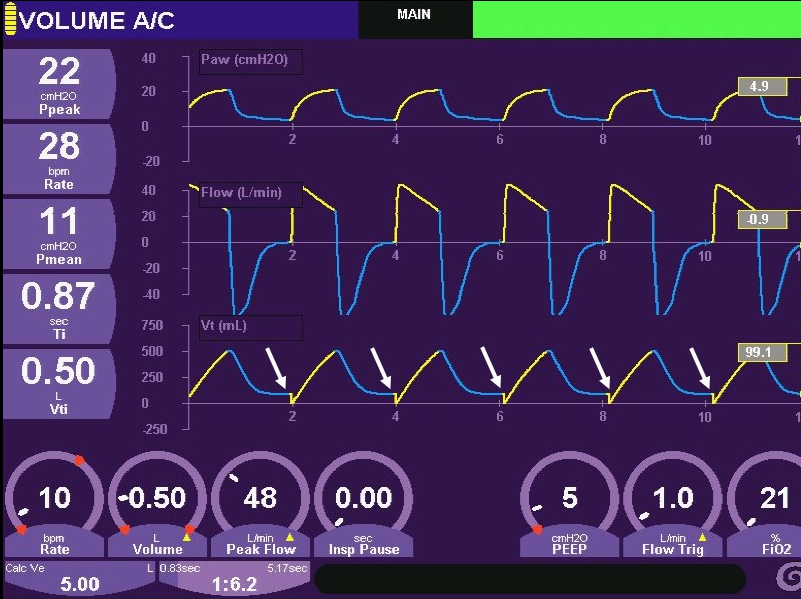
Pressure flow and volume graphics over time. Arrows indicate that returned volume less than delivered volume.
The rapid development of tachypnea in a mechanically ventilated patient can be caused by many things including sudden deterioration of the underlying disease process, circuit vibrations (eg, cardiac oscillations), triggering breaths, as well as a ventilator malfunction. The absence of significant changes in the patient’s vital signs plus the obvious leak make the diagnosis straightforward here. A stable pneumothorax (without a large bronchopleural fistula), an enlarging effusion, or acute bronchospasm will raise airway pressures in VACV and may stimulate the patient’s respiratory drive. However, this patient’s airway pressures are lower, and we have an alternative explanation for the increased respiratory rate. Reverse triggering is an interesting phenomenon whereby a patient initiates an inspiratory effort during the delivery of a controlled breath. This usually occurs in heavily sedated patients with a high control breath rate, conditions not present in this patient. Finally, one of the most common causes of an increased breathing frequency in mechanically ventilated patients is double-triggering, a situation that usually develops when neural inspiratory time is longer than the mechanical inspiratory time. The persistent effort can then result in a second triggered breath. This is not case for this patient who has a regular rapid breathing pattern.12345
You are called to see a patient who is being supported by mechanical ventilation because the high breath rate alarm has activated. The patient is receiving volume-assist control ventilation (VACV) and is recovering from a severe pneumonia. He appeared to be improving while visiting him during rounds an hour ago when his peak airway pressures were noted to be 25 cm H2O, down slightly from the previous day on similar settings. Currently, his peak airway pressure is 22 cm H2O. He is awake and responsive, and his vital signs have not changed appreciably other than the respiratory rate, which has risen abruptly from 14 (set rate of 10) to 28 breaths/min. The current ventilator graphics are shown. What is likely occurring?
Links to this note
Footnotes
-
Brochard L, Martin GS, Blanch L, et al; Clinical review: Respiratory monitoring in the ICU - a consensus of 16. Crit Care. 2012;16(2):219. PubMed ↩
-
MacIntyre NR. Respiratory system mechanics. In: MacIntyre NR, Branson RD, eds. Mechanical Ventilation. 2nd ed. Philadelphia, PA: WB Saunders; 2008:159-170. ↩
-
Marini JJ, Rodriguez M, Lamb V. Bedside estimation of the inspiratory dynamics relevant to mechanical ventilation. Chest. 1986;89:56-62. ↩
-
Truwit JD, Marini JJ. Evaluation of thoracic mechanics in the ventilated patient. J Crit Care. 1988;3:133-150;192-213. ↩