lymphocyte predominant pleural fluid suggests lymphoma, TB, ESRD
- related: pleural effusion
- tags: #literature #pulmonology
ESRD patients can have transudate effusion that’s lymphocyte predominant
This patient has multiple risk factors for Mycobacterium tuberculosis infection (TB) and pleural studies concerning for tuberculous pleural effusion. Among patients with tuberculous pleural effusion, 40% to 85% will also have parenchymal lung involvement; therefore, it is important to evaluate for active lung disease and take appropriate infection control measures.
The prevalence of tuberculous pleural effusion varies based on geography and can represent 3% to 20% of extrapulmonary TB cases. Risk factors for tuberculous pleural effusions are older age, HIV positivity, and other causes of immunocompromised status. Tuberculous pleural effusions are believed to arise either from delayed hypersensitivity reaction to TB or as a direct result of M tuberculosis infection in the pleural space. M tuberculosis may access the pleural space via hematogenous spread, extension from lymphatic involvement, or direct spread to the pleural space through rupture of infected lung. Initial neutrophilic immune response is followed by influx of lymphocytes into the pleural space. Interferon (IFN)-γ produced by lymphocytes leads to an effective inflammatory response that may cause the pleural effusion to resolve without antituberculous therapy in a subset of patients over the course of weeks. However, many of these patients may later develop reactivated M tuberculosis infection.
While tuberculous pleural effusions are not uncommon globally, empyema is a rare complication of tuberculous pleural effusion. Clinically, patients with tuberculous pleural effusions present acutely with fevers, pleuritic chest pain, and cough and may endorse night sweats or weight loss. Patients with empyema have a more subacute clinical presentation as tuberculous empyema may develop over several months in the setting of an existing tuberculous pleural effusion. Tuberculous pleural effusions and empyema are typically unilateral and loculated, and empyema often has a classic radiographic finding of a calcified or thickened pleural lining.
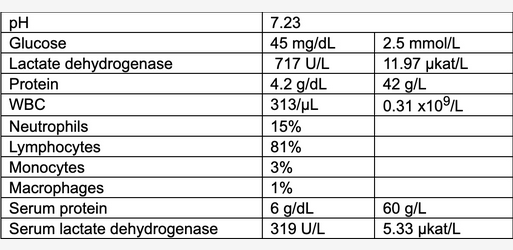
Pleural fluid studies are exudative based on Light’s criteria (pleural fluid protein-to-serum fluid protein ratio >0.5, pleural fluid lactate dehydrogenase [LDH]-to-serum fluid LDH ratio >0.6, or pleural fluid LDH greater than two-thirds the upper limit of normal), and up to 90% of cases are lymphocyte predominant. Globally, the most common cause of lymphocytic pleural effusion is M tuberculosis. Differential diagnosis includes malignancy, chylothorax, rheumatoid arthritis, postcardiac surgery, primary effusion lymphoma, sarcoidosis, yellow nail syndrome, and Erdheim-Chester disease.
While malignancy is on this differential diagnosis and should be considered in a patient with unintentional weight loss, the best next step would be to take appropriate infection control measures while pursuing definitive diagnosis from a differential that includes active pulmonary tuberculosis. Bacterial pneumonia typically causes neutrophil-predominant pleural effusion or empyema. IFN-γ release assay detects cell-mediated immune response to mycobacterial peptides. The test can be positive in nontuberculous mycobacterial infections, and a negative test does not rule out active TB. Given the high pretest probability of TB in this patient, the results of an IFN-γ release assay would not be helpful in clinical decision-making.123456
A 52-year-old patient with no medical history comes to the emergency department for dyspnea. She works at a migrant shelter and volunteers abroad every summer. She recently returned from a 3-month volunteering trip to India. For the past 3 weeks, she has experienced right-sided pleuritic chest pain, nonproductive cough, 4 lb (1.81 kg) weight loss, and shortness of breath after walking one block.
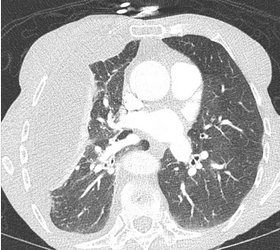
In the emergency department, the patient’s temperature is 38.3 °C; SpO2 is 91% while breathing room air; pulse is 95/min; respirations are 34/min; and BP is 130/85 mm Hg. Physical examination is notable for tachypnea and diminished breath sounds in the right lung field. A chest radiograph is obtained, followed by CT scan of the chest (Figure 1). The patient is placed on high-flow nasal cannula oxygen and admitted to the ICU out of concern for impending respiratory failure. Ultrasonography of the right hemithorax shows a 6-cm area of anechoic fluid above the diaphragm with complex septations. Diagnostic thoracentesis is performed at the bedside and yields 100 mL cloudy fluid. Laboratory values for pleural fluid analysis are shown in Figure 2.
Based on the pleural fluid analysis results, which of the following is the most important next step?
Links to this note
Footnotes
-
Baumann MH, Nolan R, Petrini M, et al. Pleural tuberculosis in the United States: incidence and drug resistance. Chest. 2007;131(4):1125-1132. PubMed ↩
-
D’Annunzio S, Felner K, Smith RL. Go with the flow: an elderly man with a pleural effusion. Ann Am Thorac Soc. 2016;13(11):2078-2081. PubMed ↩
-
McNally E, Ross C, Gleeson LE. The tuberculous pleural effusion. Breathe (Sheff). 2023;19(4):230143. PubMed ↩
-
Sahn SA, Iseman MD. Tuberculous empyema. Semin Respir Infect. 1999;14(1):82-87. PubMed ↩
-
Zhai K, Lu Y, Shi HZ. Tuberculous pleural effusion. J Thorac Dis. 2016;8(7):E486-E494. PubMed ↩