Malaria causes cyclic fevers
- related: Infectious Disease ID
- tags: #literature #pulmonology
This patient with recent travel to Sub-Saharan Africa has an acute-onset febrile illness, scleral icterus, mild splenomegaly, anemia, and thrombocytopenia. This presentation is most consistent with malaria.
Plasmodium falciparum accounts for the majority of deaths from malaria, followed by Plasmodium vivax. Many of the clinical symptoms seen in malaria are due to the infected parasite-containing red blood cells adhering to nearby vessels, causing small infarcts, leakage of capillaries, and, ultimately, organ dysfunction. Diagnosis is confirmed with examination of a peripheral blood smear looking for trophozoites.
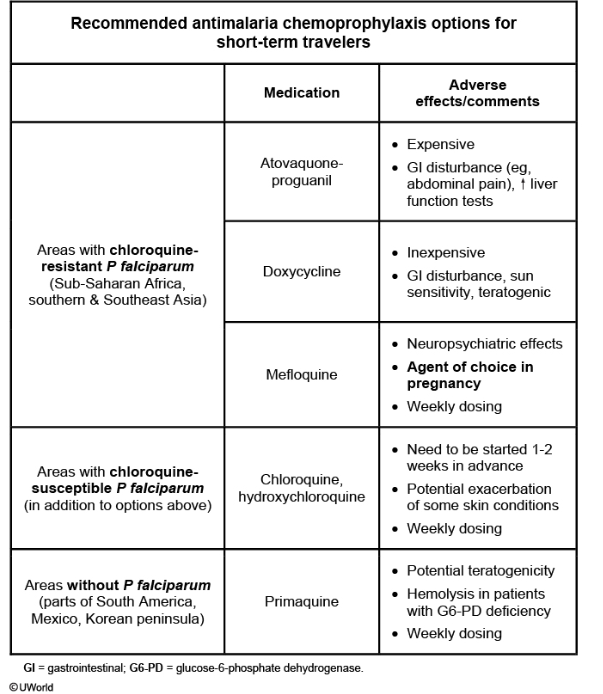
Commonly used malaria prophylaxis drugs (eg, chloroquine, mefloquine, and doxycycline) target the blood stage of the parasite (blood schizonticides) when released from the liver. Tissue schizonticides (eg, atovaquone/proguanil) are designed to target the liver stage, where the parasites grow and can stay dormant in the liver (or other tissues). The blood schizonticides must be continued for at least 4 weeks after leaving an endemic area to ensure eradication of parasites released from the liver.
This patient did take doxycycline for malaria prophylaxis but discontinued his medication on return to the United States, causing it to be ineffective.1
This patient’s presentation is typical of and will be diagnosed by a properly prepared and analyzed blood smear (Figure 2) (choice B is correct). The evaluation of fever in a returning traveler should always include malaria because it can progress to severe malaria as seen in this case. This case emphasizes the progression of disease caused by the delay in diagnosis from not considering malaria earlier in the patient’s course. The patient should have received a rapid diagnostic test and thin and thick smears early in the presentation and treatment with oral agents such as artemether-lumefantrine. By the time he was admitted, he had progressed to severe malaria, which includes findings such as an elevated parasitemia on peripheral smear, renal failure, impaired consciousness, prostration, convulsions, lactic acidosis, severe anemia, elevated bilirubin levels (not isolated elevation as in leptospirosis), splenic enlargement, pulmonary edema, bleeding from gums or venipuncture sites, and shock. At this point, he now requires ICU admission and will need to be treated with IV artesunate in coordination with an infectious disease consultation. Until May 2022, IV artesunate required an Investigational New Drug approval and distribution from the Centers for Disease Control and Prevention. In 2022, it was approved by the Food and Drug Administration, but it is still difficult to obtain this IV drug, which is necessary for this patient’s manifestation of severe malaria.
This patient has returned from Honduras, which has an incidence of more than 90% of malaria cases caused by Plasmodium vivax, a less virulent cause of malaria. Unfortunately, this patient contracted disease caused by Plasmodium falciparum, a more virulent malarial form more likely to progress to severe malaria if untreated. There are five species of Plasmodium that cause human disease: P falciparum, P vivax, Plasmodium ovale, Plasmodium malariae, and Plasmodium knowlesi. P falciparum is the species associated with the most severe clinical presentation and is responsible for the majority of malaria deaths. The other strain in Honduras, P vivax, is associated with a less severe course but has been associated with relapse that can occur months later.
One other disease process common to Honduras but not listed as an option is Dengue. Dengue is transmitted by the day-biting Aedes mosquito and will manifest as a febrile illness with nonspecific symptoms such as malaise and “breakbone fever,” which is the presence of significant arthralgia. Patients with severe hemorrhagic Dengue can exhibit visible petechiae. Dengue is very common in Honduras and certainly would be a consideration in this patient’s presentation. Nonetheless, malaria must be excluded.
Although 50% of patients with malaria may have minor symptoms of diarrhea (perhaps from coinfections related to travel), many of this patient’s findings point away from GI disease as a likely explanation for his progression to critical illness (choice A is incorrect). Enterotoxigenic Escherichia coli is classically associated with traveler’s diarrhea, which produces profuse watery diarrhea and severe abdominal cramps. Aside from the diarrhea component, however, presentation of typical enterotoxigenic E coli infection would not be consistent with this patient’s multisystem organ dysfunction and cyclical fevers.
Leptospirosis causing severe disease is usually associated with jaundice and marked elevations of bilirubin levels. Although leukopenia, thrombocytopenia, and renal failure occur in leptospirosis, hypoglycemia is more typical of malaria (choice C is incorrect). A significant risk factor for leptospirosis is freshwater exposure with small mammal urine contamination, which would be possible here, but malaria is more likely with travel in Honduras.
Typhoid fever is caused by Salmonella typhi or Salmonella paratyphi and is less likely than malaria as a cause of fever and multisystem organ failure in travelers to Honduras. Rash in patients with typhoid is described as a rose spot, and typhoid can be diagnosed by recovering the organism from blood, skin biopsy, or bone marrow biopsy specimens with culture (choice D is incorrect). Typhoid can cause life-threatening systemic infection, but leukopenia would be very unexpected in an immunocompetent host.2