Management of Life-Threatening Asthma
- related: Asthma reactive airway disease
- tags: #literature
- source: pubmed1
Asthma exacerbation
- peak expiratory flow or FEV1 less than 50-60% predicted signals severe exacerbation
- lack of FEV1 flow rate improvement after initial bronchodilator therapy suggests need for hospitalization
Airway
- HFNC: no improvement in clinical response compared to conventional O2.
- Bipap
- start at EPAP 5 and IPAP 10
- Bag mask
- can worse hyperinflamation, barotrauma, acidosis can increase demand and lead to arrest, dynamic instability
- Intubation
- always consider asthma patients as difficult airway
- Use large tube > 8mm to relieve airway resistance
- Use delayed sequence intubation separating induction from analytics
- Use elevated shock index can suggest shock to for preemptive resuscitation if shock index > 1
- Ketamine is preferred as it does not cause hemodynamic instability
- Barotrauma
- pneumothorax and pneumomediastinum common result of high pressures
- Ventilator strategies
- target low initial respiratory rate (8-10 breaths)
- TV 6-8cc/kg
- allow hypercarbia with PaCO2 90-100 mHg
- permissive acidosis pH > 7.2
- decrease inspiratory time to avoid breath stacking
- I:E higher than 1:2, can use 1:3 or 1:4
- disconnect from vent if still breath stacking and compress chest for 30-60s
- match auto peep with extrinsic PEEP but don’t set extrinsic PEEP too high
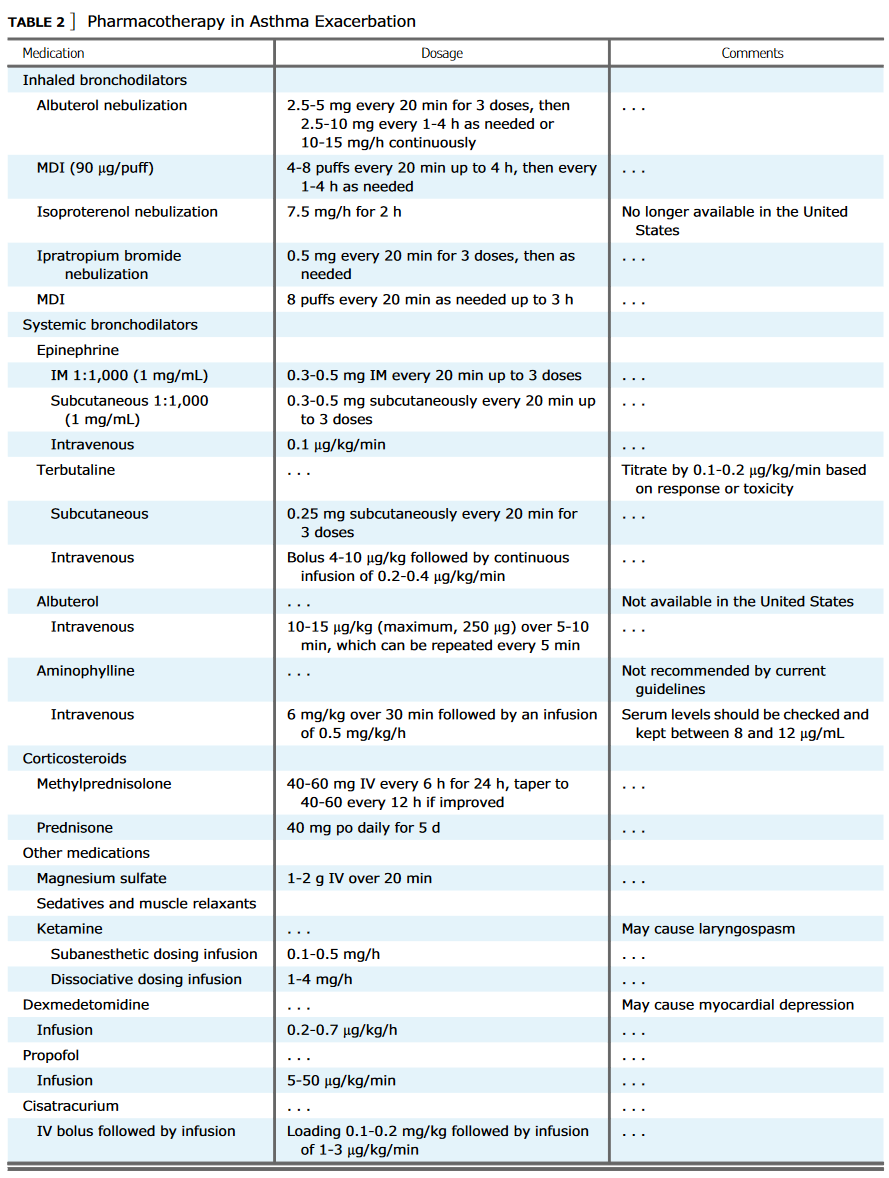
Initial Treatment
- SABA
- continuous albuterol or intermittent dosing are first line agents
- higher dose7.5 mg offers no benefit over 2.5 mg dosing
- full agonists (formoterol and isoproterenol) have superiority than albuterol but can have higher side effects
- Steroids
- start as soon as possible
- takes 6-12h to start working
- no significant difference between PO and IV
- IV methylprednisolone recommended as starting steroids (steroid equivalents)
- Mag
- magnesium sulfate inhibits calcium channel and blocks parasympathetic tone
- improves PFT and reduces hospital admission but not mortality
Life Threatening Acute Exacerbation
- Consider IM vs SQ epinephrine but can cause hypokalemia and tachyarrhythmia
- Heliox
- improves PEF in severe (PEF >50%) and very severe (PEF < 50% pred) exacerbation
- FiO2 needs to be < 30% to be used properly
- stop if no response in 15 min
- Inhaled anesthetics
- can be used to avoid high peak pressure, hypercarbia
- isoflurane/halothane reduces bronchospasm
- need special anesthesia ventilator
- NMB: use boluses and avoid infusion to prevent myopathy
- Nimbex: initial 0.1-0.2 mg/kg bolus, followed by 0.03 mg/kg bolus each hour after