MDR pseudomonas treatment includes cefiderocol
- related: Infectious Disease ID
- tags: #literature #id
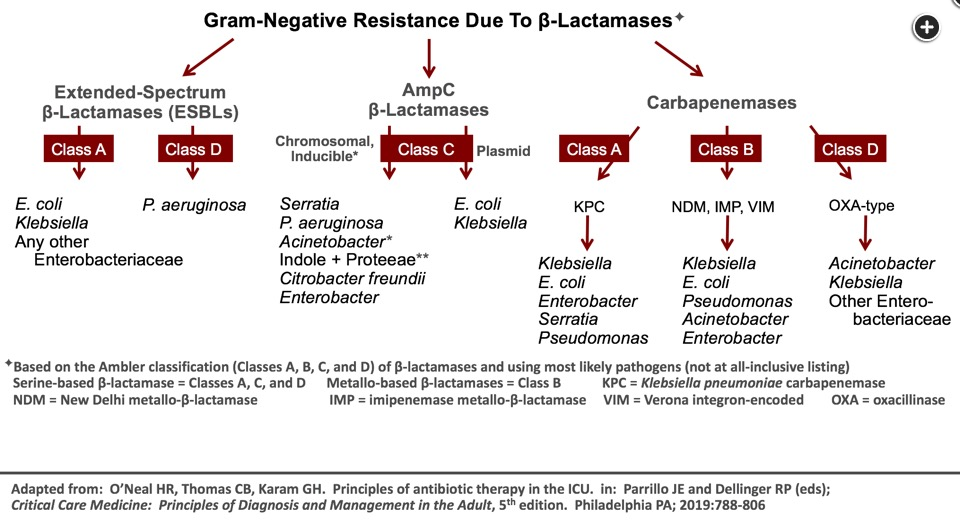
This patient meets the definition of complicated urinary tract infection based on the structural abnormalities in his kidney from not only his polycystic kidney disease but also his obstructive uropathy. Epidemiologically, he is at risk for all three of the clinically important patterns of resistance to β-lactam antibiotics: (1) extended-spectrum β-lactamase (ESBL) production by gram-negative Enterobacteriaceae like Escherichia coli and Klebsiella pneumoniae, (2) carbapenem-resistant P aeruginosa, and (3) carbapenemase-producing bacteria with a serine structure ((ie, the Ambler A eg, K pneumoniae carbapenemases (KPCs) or Ambler D (eg, OXA-like)) β-lactamase or with a metallo structure (ie, Ambler B (eg, NDM, VIM, IMP)) β-lactamase. These are depicted in the accompanying concept map (Figure 1). With his clinical presentation of septic shock and his risk factors for multiple mechanisms of resistance (including his recent 6-month residence in Asia and Eastern Europe, where NDM and OXA β-lactamases are prevalent), antimicrobial therapy should be selected with emphasis on coverage for as many of the resistance mechanisms as possible.
For β-lactam antibiotics to travel to their site of action, which are penicillin-binding proteins that are responsible for synthesis of the bacterial cell wall, they must first enter the bacterial cell. Porins are trimeric proteins that are located in the outer membrane of the bacterial cell wall and allow antibiotics to enter bacteria through passive diffusion. When these porins close, the bacterial cell wall becomes less permeable, and the result is less antibiotic reaching the target site of action (ie, penicillin-binding proteins). Porin channel closure is a classic mechanism of carbapenem resistance in P aeruginosa. To overcome the issue of impermeability in gram-negative bacteria, including those that are carbapenem resistant, additional entry sites in the bacterial cell wall have been studied. One of those is the iron transport system, which, like porins, is located in the outer membrane of the bacterial cell wall. The iron transport system exists in response to the need that most organisms have for iron as an essential element for growth. To facilitate the acquisition of iron, bacteria secrete small, high-affinity iron-chelating compounds called siderophores. Once these siderophores have scavenged iron, they carry it back into the bacteria through the iron transport system, which is an active process in contrast to the passive diffusion that occurs when porin channels are used for antibiotic entry. Cefiderocol is the combination of a cephalosporin antibiotic and a catechol moiety, with the latter functioning to bind extracellular free iron that can be used for bacterial growth. Acting as a siderophore, the cefiderocol-iron combination travels to the bacterial cell and unlocks the iron transport system, allowing entry into the bacterial cell wall and the subsequent journey of the antibiotic component to penicillin-binding proteins. This has been characterized by some as using the Trojan horse approach to gain entry into the bacteria. A noteworthy property of cefiderocol is its stability in the presence of β-lactamases represented in all four of the Ambler classes, including serineand metallo-based carbapenemases. In addition, it is a poor substrate for efflux pumps, which extrude certain antibiotics from the periplasmic space before they can reach the penicillin-binding proteins. As such, cefiderocol is stable in the presence of the three classic mechanisms of gram-negative resistance to carbapenems: inactivation by β-lactamases, impermeability, and efflux.
The MERINO trial was an international, multicenter, open-label, noninferiority, randomized controlled trial comparing piperacillin/tazobactam to meropenem for the definitive treatment of bloodstream infections caused by third-generation cephalosporin-nonsusceptible E coli or Klebsiella species (with that resistance pattern being a marker for ESBL production). The trial enrolled 379 patients from 26 sites in nine countries, with 30-day mortality as the primary end point. More than 50% of the enrolled patients had health care-associated infections, with the urinary tract as the most common site (60.9%) and E coli as the most common organism (86.5%). There was a statistically significant difference in mortality rate in patients treated with piperacillin/tazobactam (in 23 patients, 12.3%) compared with meropenem (in seven patients, 3.7%). There was no difference between the two groups either with subsequent infections due to drug-resistant bacteria or with Clostridium difficile infection. This study did not support the use of piperacillin/tazobactam for bloodstream infections caused by ESBL-producing bacteria. Because of the severity of this patient’s illness and the risk for ESBL-producing E coli or K pneumoniae, piperacillin/tazobactam would not be the favored agent.
Ceftolozane/tazobactam is stable in the presence of all three of the chromosomally mediated mechanisms of resistance in P aeruginosa. In addition, it has in vitro activity against ESBL-producing Enterobacteriaceae. It is not active in the presence of either the serine carbapenemases (ie, KPCs or OXAs) or the metallo carbapenemases (ie, NDMs), for which the patient is at risk since he resided in an area endemic for organisms with these resistance mechanisms for the past 6 months and had significant prior antibiotic exposure.
This patient’s P aeruginosa isolate from his previous episode of urosepsis was not susceptible to meropenem. A shortcoming of the β-lactamase inhibitor vaborbactam is that adding it to meropenem does not result in a significant increase in P aeruginosa susceptibility to meropenem. Meropenem/vaborbactam does have activity against KPCs, but it is not active against bacteria producing the metallo NDM β-lactamases.1234
Links to this note
Footnotes
-
Harris PNA, Tambyah PA, Lye DC, et al; MERINO Trial Investigators and the Australasian Society for Infectious Disease Clinical Research Network (ASID-CRN). Effect of piperacillin-tazobactam vs meropenem on 30-day mortality for patients with E coli or Klebsiella pneumoniae bloodstream infection and ceftriaxone resistance: a randomized clinical trial. JAMA. 2018;320(10):984-994. PubMed ↩
-
Kramer J, Özkaya Ö, Kümmerli R. Bacterial siderophores in community and host interactions. Nat Rev Microbiol. 2020;18(3):152-163. PubMed ↩
-
Zhanel GG, Golden AR, Zelenitsky S, et al. Cefiderocol: a siderophore cephalosporin with activity against carbapenem-resistant and multidrug-resistant gram-negative bacilli. Drugs. 2019;79(3):271-289. PubMed ↩