methemoglobinemia has reduced O2 saturation with normal PaO2
- related: Step 3, Medicine, General Medicine, ICU intensive care unit
- tags: #literature #pulmonology #icu
Vs Others
- venous hyperoxia differentiates between methemoglobinemia and cyanide toxicity
- hypoxia differentiates between LAST and methemoglobinemia
Pathophysiology
Causes
Symptoms and Clues to Diagnosis
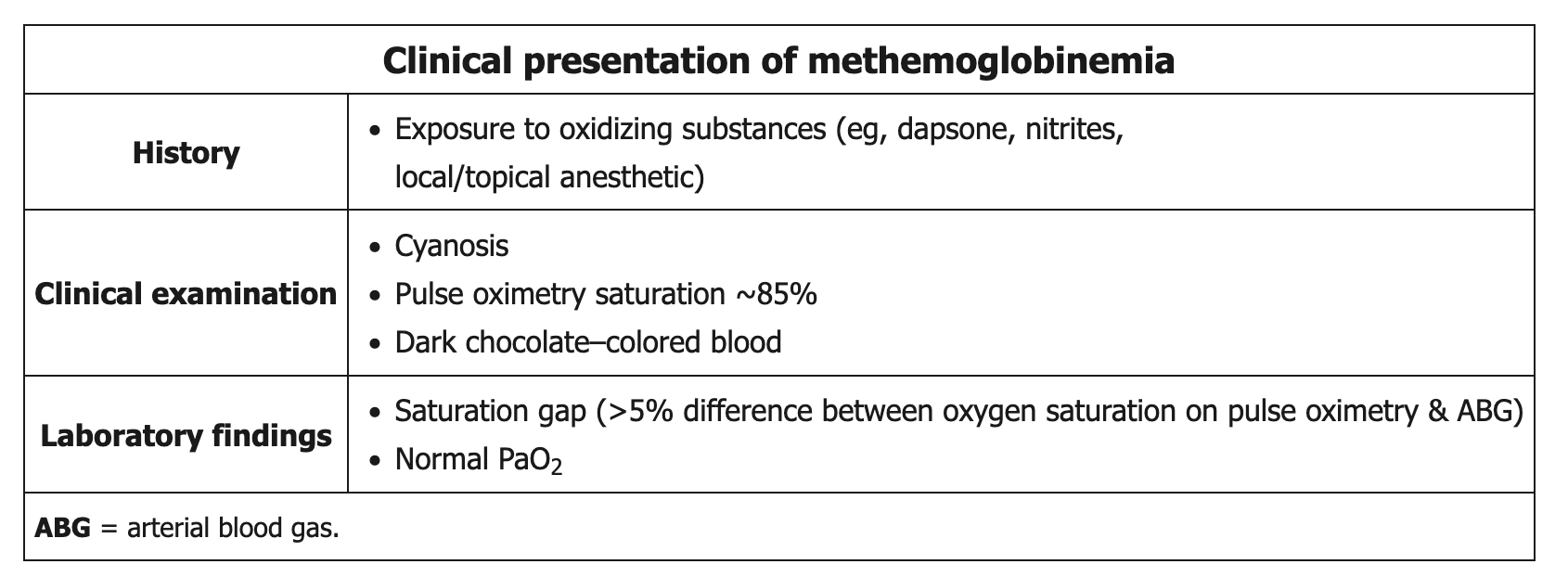
The fact that low SpO2 remains low despite maximum high-flow nasal oxygen raises concerns for right-left shunt and methemoglobinemia. Measurement of PaO2 of 280 mm Hg excludes sufficient shunting to produce SpO2 of 84%. The high oxygen saturation gap (>5%) between calculated blood oxygen saturation (99% for PaO2, 280 mm Hg in this case) vs oxygen saturation via pulse oximetry (84% in this case) raises concern regarding presence of a dyshemoglobinemia, which can be detected by using cooximetry of arterial blood. In contrast to measuring only light wavelength corresponding to oxyhemoglobin and deoxyhemoglobin with pulse oximetry, cooximetry uses four or more light wavelengths to calculate percentages of methemoglobin, carboxyhemoglobin, oxyhemoglobin, and deoxyhemoglobin in arterial blood.
Patients typically have cyanosis and dark chocolate-colored blood. Standard pulse oximetry readings are low (85%) due to the absorption spectrum of methemoglobin and do not represent the true oxygen saturation.
The clue to the diagnosis is the reduced oxygen saturation with normal Pao2, and the diagnosis can be confirmed with cooximetry, measuring oxyhemoglobin, deoxyhemoglobin, carboxyhemoglobin, and methemoglobin (MetHb) as a percentage of total hemoglobin. Pulse oximetry is inaccurate in the diagnosis of methemoglobinemia, as the peak absorbance of that molecule is at 631 nm, while pulse oximetry estimates oxygen saturations at wavelengths of 660 nm and 940 nm. Pulse oximeters may initially read falsely high oxyhemoglobin levels, but when MetHb levels reach around 30%, the oximeter tends to read the oxygen saturation at a consistent value of around 85%, as in this patient. Patients usually develop cyanosis at MetHb levels of around 15%, symptoms at around 30%, and mental status changes at around 50%. MetHb levels exceeding 70% are usually fatal.
Due to the poor oxygen affinity of methemoglobin, the administration of supplemental oxygen does not improve cyanosis, blood color, or pulse oximetry readings. Because arterial blood gas testing analyzes unbound arterial oxygen (as opposed to hemoglobin-bound oxygen), the PaO2 is normal and overestimates the degree of true oxygen saturation. With severe cases of methemoglobinemia, the decreased oxygen delivery can result in altered mental status, seizures, and death.
Confirmation of the diagnosis requires a co-oximeter, which is a device that can accurately measure the presence of methemoglobin. The offending agent(s) should be discontinued in all patients with suspected methemoglobinemia, while symptomatic patients and those with a methemoglobin level > 20% require prompt administration of methylene blue (a reducing agent). Those in shock may also require blood transfusion or an exchange transfusion.
Diagnosis
Treatment
Treatment is usually indicated for methemoglobin levels >30%. Methylene blue is a cofactor of nicotinamide adenine dinucleotide phosphate (NADP)-MetHb-reductase and increases the capacity of the enzyme to reduce ferric iron levels. The usual dose is 1 to 2 mg/kg over 5 min; methylene blue may increase MetHb levels in doses >15 mg/kg and in patients with glucose-6-diphosphate deficiency.1
Treatment: Methylene blue acts as an electron acceptor for NADPH and is reduced to leucomethylene blue, which in turn reduces methemoglobin back to hemoglobin.2
Fomepizole is an inhibitor of alcohol dehydrogenase used in the treatment of methanol and ethylene glycol toxicity by reducing generation of toxic metabolites. Sodium nitrite and sodium thiosulfate are used as antidotes to cyanide poisoning through increasing methemoglobin levels to facilitate transport of cyanide as cyanomethemoglobin from mitochondrial cytochromes to hepatocytes. Heparin would be given to a patient with postoperative pulmonary embolism, but oxygen desaturation by pulse oximetry with a normal Pao2 would not occur in that condition.
This patient exhibited low oxygen saturation on pulse oximetry—a situation that should initiate a logical approach to stabilize the patient and detect treatable causes. The first step is to determine whether the patient is in respiratory distress and requires urgent escalation of care. The patient has minimal symptoms, is alert, has acceptable vital signs, and has a PaO2 of 280 mm Hg. Accordingly, endotracheal intubation and invasive ventilation to provide FiO2 of 1.0 is not indicated (choice A is incorrect).
Regarding the cause, this patient could be at risk of experiencing deterioration in oxygenation as a result of pulmonary edema due to rapid infusion of normal saline to treat TLS or acute exacerbation of COPD. However, the absence of supporting evidence on examination and imaging makes these conditions unlikely, as does the presence of high PaO2. Continuous nebulized albuterol would not be an effective treatment (choice B is incorrect).
You are evaluating a 60-year-old man of Mediterranean descent who has newly diagnosed diffuse large B-cell lymphoma and tumor lysis syndrome (TLS) and now has a decrease in SpO2 via pulse oximetry from 96% to 84% while breathing 2 L/min O2 via nasal cannula. He has underlying COPD treated with a long-acting muscarinic antagonist/long-acting β-agonist inhaler. While at an outside hospital yesterday, he was noted to be in TLS with a uric acid level of 12.0 mg/dL (0.71 mmol/L); he also had suspected hemolysis with increased lactate dehydrogenase, low haptoglobin, and a decrease in hemoglobin from 13 g/dL (130 g/L) to 10.5 g/dL (105 g/L). A glucose-6-phosphate dehydrogenase level was obtained at the outside hospital.
Just prior to transfer yesterday, he was started on a rapid infusion of normal saline and received allopurinol and rasburicase for TLS. Now he complains of mild dyspnea and fatigue but is otherwise asymptomatic. Examination reveals a heart rate of 90/min, a respiratory rate of 18/min, a BP of 130/85 mm Hg, and SpO2 of 84% (with excellent waveform). He has good air movement and normal breath sounds without wheezing or crackles. He has mild lip cyanosis, normal cardiac examination findings, and trace pretibial edema. His nasal oxygen was increased to 6 L/min and then replaced with high-flow nasal oxygen, which was escalated to 50 L/min and 100% oxygen without significant improvement in SpO2. A chest radiograph demonstrates moderately hyperinflated lungs only. An arterial blood sample with the following appearance (Figure 1) has the following arterial blood gases: pH 7.41, PCO2 42 mm Hg, and PO2 280 mm Hg. Co-oximetry is ordered, and TLS treatment is discontinued.

Which of the following interventions should be performed at this time?
A 52-year-old man is admitted with hematemesis. He has been taking ibuprofen several times daily for the past week after a back injury but otherwise has no significant medical history and takes no other medications. Esophagogastroduodenoscopy is performed, revealing a bleeding gastric ulcer; hemostasis is achieved after clip placement. Shortly after the procedure, the patient has a low Spo2 and subsequently has a generalized tonic-clonic seizure. Lorazepam is administered with resolution of the seizure; the patient then undergoes intubation for persistently low SpO2. His vital signs include a temperature of 37.6 °C, heart rate of 87/min, BP of 123/68 mm Hg, respiratory rate of 16/min, and SpO2 of 84%; ventilator settings are tidal volume of 400 mL, PEEP of 5 cm H2O, respiratory rate of 16/min, and FIO2 of 1.0. Arterial blood gas measurements show a pH of 7.32, PCO2 of 38 mm Hg, and PO2 of 347 mm Hg. A chest radiograph reveals appropriate placement of the endotracheal tube and is otherwise within normal limits.
Links to this note
-
venous hyperoxia differentiates between methemoglobinemia and cyanide toxicity
-
use ascorbic acid to treat methemoglobinemia in G6PD deficient patients