monkeypox aka mpox has rash and
- related: Infectious Disease ID
- tags: #literature #pulmonology
The history of this patient and the skin findings strongly suggest a presentation of mpox, formerly known as monkeypox, in an immunocompromised patient. The recommended antiviral treatment in this setting is tecovirimat.
Mpox is caused by an orthopox DNA virus that is in the same genus as variola (the etiologic agent of smallpox) and varicella. In prior decades infections due to mpox were almost entirely limited to endemic areas of Africa, but in 2022 an outbreak with person-to-person transmission spread to 16 countries, including the United States and Europe. In early reports characterizing this outbreak, over 95% of the patients were men who had sex with men. Almost all patients presented with a rash, commonly in the anogenital area but occasionally more widely spread as in this patient. The lesions may be macular, pustular, vesicular, or crusted and often exhibit varying stages of development. Spread to mucosal surfaces is common as is regional lymphadenopathy. Early diagnosis can be made by polymerase chain reaction assay of specimens recovered from involved tissues.

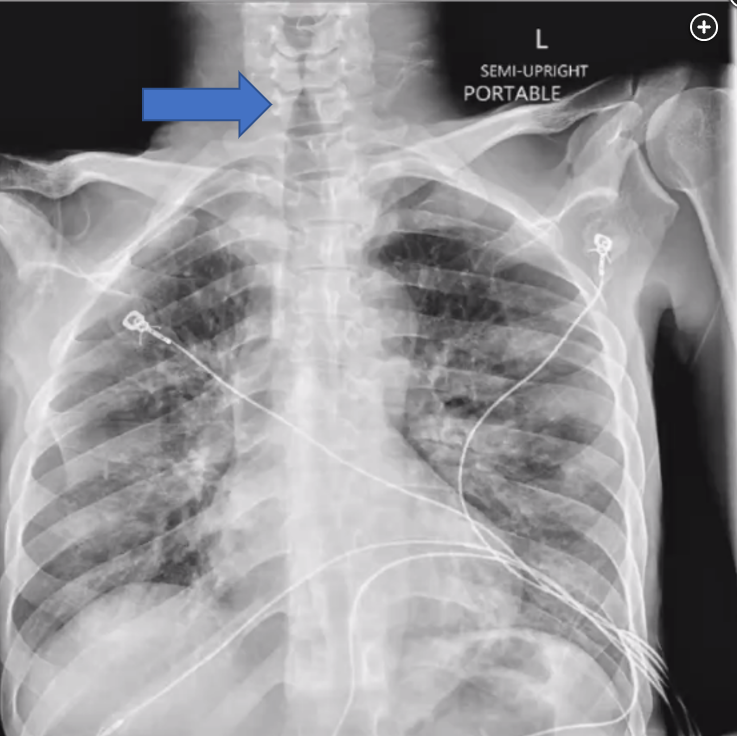
In most cases mpox infection is managed on an outpatient basis and is self-limited with a mortality much lower than variola virus infection. Supportive treatment is required for pain control and to avoid secondary bacterial infection of skin lesions. A small fraction of patients will become critically ill and thus familiarity with this disorder is advisable for pulmonary and critical care physicians. Causes of critical illness from this viral infection include underlying immunosuppression, wide dissemination, encephalitis, and involvement of the upper airway. The patient described here had a low CD4 count and high HIV viral load related to nonadherence to HIV therapy. Involvement of the pharynx and epiglottis with impending complete upper airway obstruction was strongly suggested by the patient’s history and physical examination findings. In addition, the chest radiograph obtained in the ED exhibited a steeple sign (see Figure 4, large arrow). Although the steeple sign may be caused by normal closure of the vocal cords, in this case severe obstruction of the upper airway was observed at the time of fiberoptic intubation and further characterized by postintubation imaging (see Figure 5, large arrow).
Although the majority of patients with mpox do not require antiviral therapy, patients as sick as the individual described here should receive antiviral treatment. Antiviral treatment is recommended for severely ill patients or for patients whose immune status makes progression likely. The patient presented has both of these broad indications. The current recommended first-line antiviral therapy is with tecovirimat, a drug developed for treatment of smallpox that inhibits a protein required for viral assembly by this genus of orthopox. At the time of this publication tecovirimat drug therapy requires Centers for Disease Control and Prevention approval. Oral and intravenous preparations are available, and a typical course is 14 days. If tecovirimat is not available, cidofovir is considered a second-line therapy, but its toxicity is significantly greater than that of tecovirimat.
An important aspect of maintaining a low threshold of suspicion for infections such as mpox is to facilitate implementation of the proper infection control measures within minutes of encountering the patient. This paradigm has been termed the identify, isolate, and inform approach and has been honed in the wake of Ebola and the Middle East respiratory syndrome outbreaks. Clearly, the opportunity for identification often begins in the ED or ICU. Because body secretions are infectious, patients with mpox require early isolation. Negative-pressure containment is required for procedures that may aerosolize virus, as in the airway management needed by this patient early in the course of his infection. Health care providers should use full personal protective equipment. Early informing of infectious disease staff and public health officials is required.
Other infections may present with prominent rashes. COVID-19 does not produce the rash shown here, so an oral agent such as nirmatrelvir-ritonavir would have no benefit (choice B is incorrect).
Fungal infections such as histoplasmosis or blastomycosis may disseminate more readily in immunocompromised hosts, but the skin lesions they produce do not have this appearance nor do these fungal infections have a predilection for spread to mucosal sites (choice C is incorrect).
Pseudomonal sepsis may present with ecthyma gangrenosum but these lesions are not so plentiful, and the individual lesion is typically a large blister with hemorrhagic or serosanguinous contents. Accordingly, antipseudomonal therapy would not be needed for this patient (choice D is incorrect).1