mucormycosis pulmonary and treatment
- related: Infectious Disease
- tags: #literature #pulmonology
Links to this note
- DM and patients on deferoxamine differentiates from aspergillosis, otherwise very similar population
- angioinvasive similar to aspergillosis
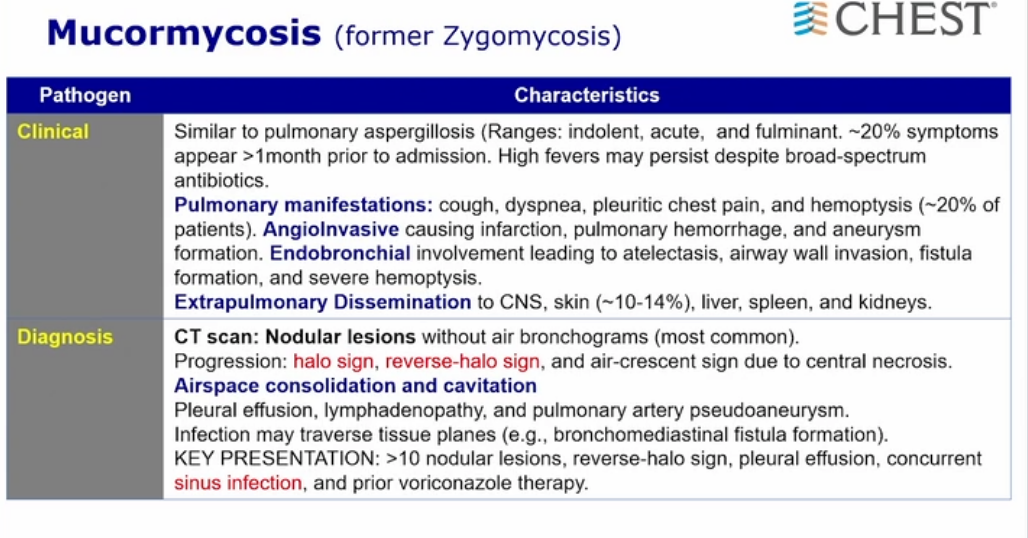
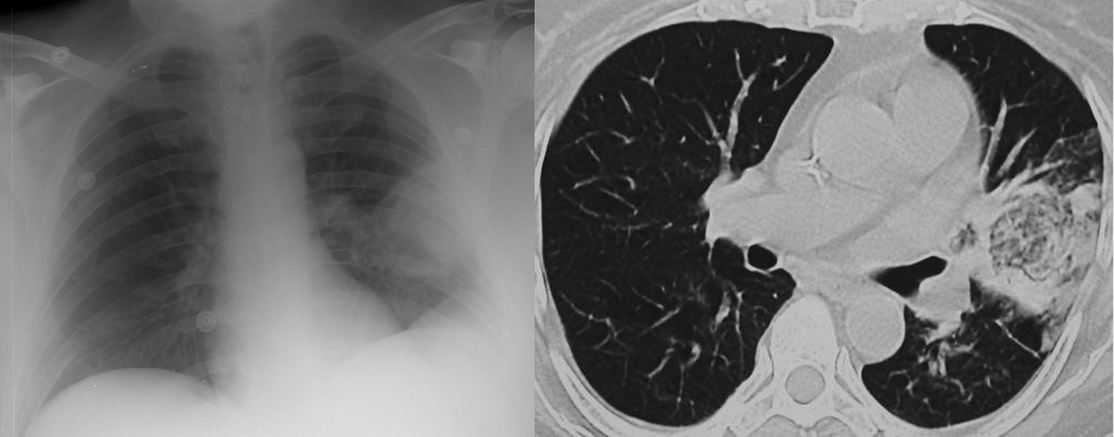
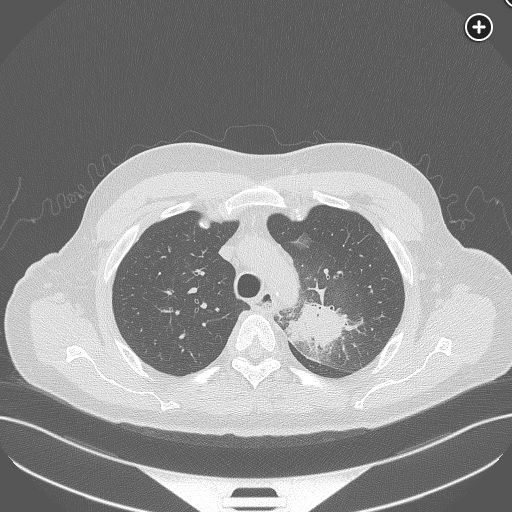
- multiple pulmonary nodules, reverse halo signs, possible pleural effusion and sinus infection
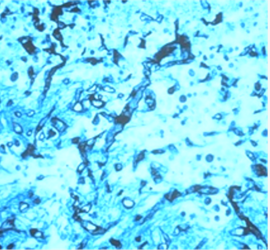
- Although more commonly observed in the setting of rhinocerebral involvement, the presence of tissue necrosis—as evidenced by black eschars, exophytic lesions and discharges—is the hallmark of invasive mucormycosis infection.


- bronchoscopy
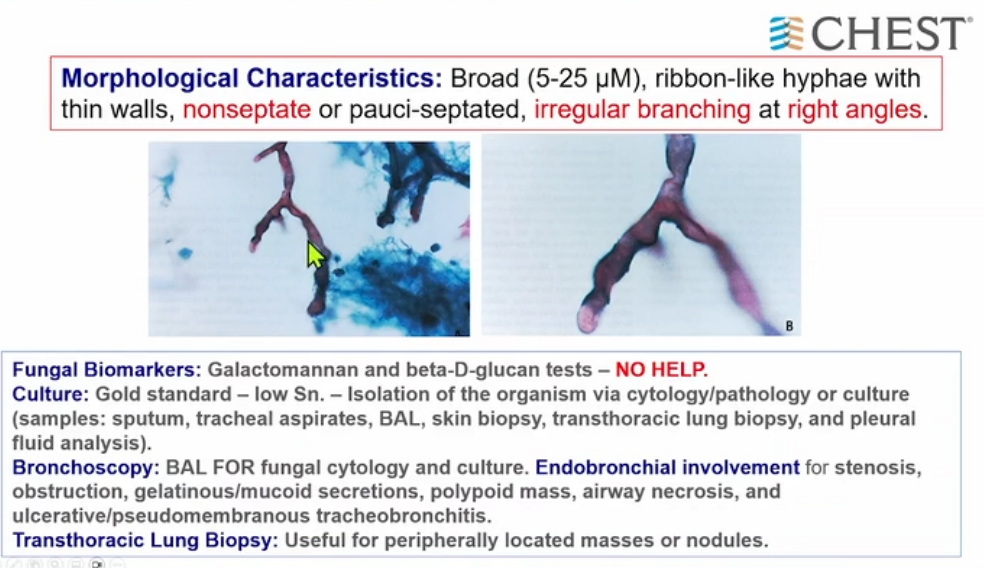
- non septated, regular branching with big angles as opposed to aspergillosis with small angles
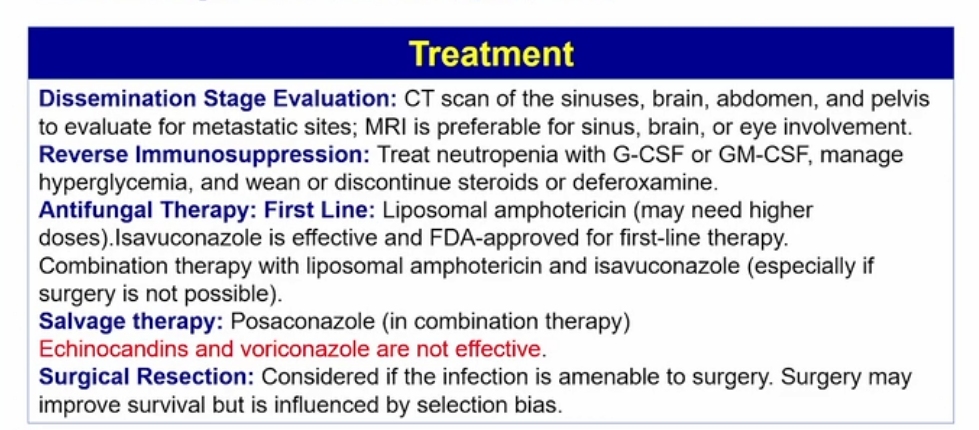
- resection if able
- medical therapy: liposomal amphotericin B
source
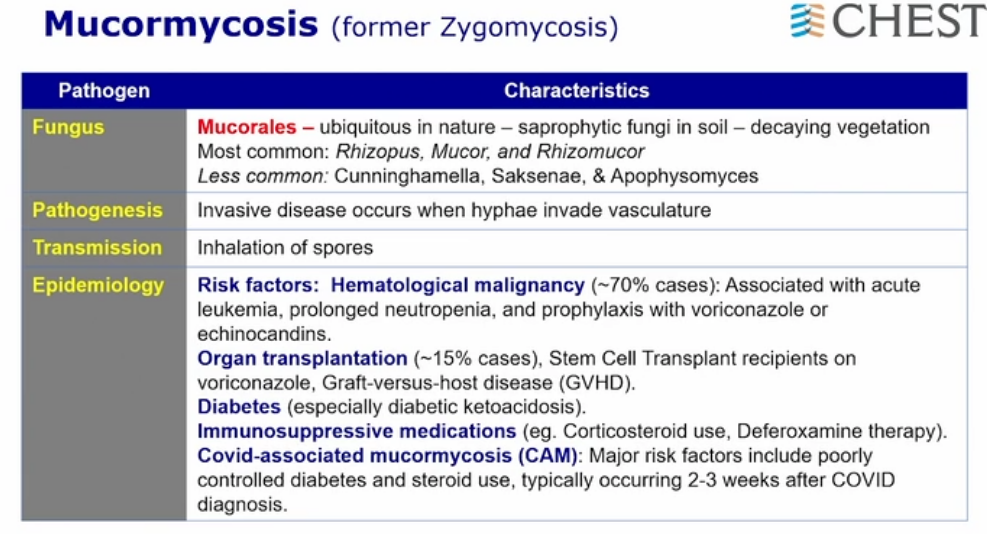
Mucormycosis is from the order Mucorales, which include the genera Rhizopus, Mucor, and Rhizomucor. The incidence of mucormycosis is significantly lower than other invasive molds, particularly, Aspergillus spp. A wide range of infection can occur, including sinus, pulmonary, central nervous system, and cutaneous infections in individuals with underlying disease. The major risks include diabetes, hematologic malignancies, hematopoietic stem cell transplantation, solid organ transplantation, iron overload, and penetrating trauma. As with Aspergillus spp. infections, prolonged neutropenia is a major risk factor. Prophylaxis with an anti-Aspergillus-based antifungal (voriconazole) may preferentially select for mucormycosis in the transplant population. Clinical presentation varies depending on syndrome, but with pulmonary or sinus disease, hemoptysis, cough, and fever are more common due to the invasive nature of the fungus. Diagnosis is optimally made with growth in fungal media, but the presence of broad-based hyphae with acute branching angles (90 degrees) on biopsy in an at-risk patient is the most common method of diagnosis.
Treatment is a combination of antifungal medication and surgery, if possible. Source control (debridement) should occur as soon as possible, but in some cases debridement may be too extensive or the patient may not be stable for surgery, as is common with hematologic malignancy patients with pancytopenia. Antifungal therapy is rarely curative but should be initiated as soon as possible. Mortality doubles for every 5 days that therapy is delayed, as antifungal therapy stops disease progression while surgical options are explored. Lipid preparation amphotericin is the drug of choice given lower administration side effects, including renal failure. If renal disease is present, therapy should not be withheld given the severity of disease, or alternative therapy should be pursued. Isavuconazonium sulfate (isavuconazole) is a good option for patients with renal disease and is well tolerated both intravenously and orally. Posaconazole is largely used as salvage therapy for patients failing amphotericin or isavuconazonium sulfate. The echinocandins (eg, caspofungin) have no activity against mucormycosis but have been described as adjuvant therapy with amphotericin in some case series. Finally, voriconazole is the treatment of choice for Aspergillus spp but has no activity against mucormycosis. No clear data exist for dual therapy (eg, liposomal amphotericin and isavuconazonium sulfate) for mucormycosis, but there are reports of use in nonsurgical candidates. Without surgical therapy, this disease is universally fatal. This patient underwent a left upper lobectomy for progressive hemoptysis, despite antifungal therapy, with eventual recovery.
Posaconazole is for salvage therapy only if liposomal amphotericin is not tolerated, but that is not the case here and the switch should not be made (choice A is incorrect). The addition of isaovuconazonium sulfate may be reasonable but not before surgical considerations (choice B is incorrect). Should this patient become too unstable for surgery, dual therapy may be tried. Finally, case reports showing the endobronchial administration of amphotericin have been reported, but no benefit has ever been described and, for that reason, it is not recommended (choice D is incorrect).1