neisseria meningoccocemia can cause purpura fulminans
- related: Infectious Disease ID
- tags: #literature #id
This patient has a clinical picture suggestive of meningococcemia, with fever and rapidly progressive septic shock, purpura fulminans, and disseminated intravascular coagulation. Acute adrenal insufficiency due to acute hemorrhagic necrosis of the adrenal glands (Waterhouse-Friderichsen syndrome) is a rare but lethal complication in this setting that often requires high index of suspicion and early empiric treatment with hydrocortisone.


There are 13 serogroups of Neisseria meningitidis, of which 6 can cause critical illness (A, B, C, W135, X, and Y). Infection is most commonly seen in children and young adults, and the distribution of serotypes tends to be specific to certain geographic regions. The “meningitis belt” of central Africa has been considered a hyperendemic area, with regular outbreaks occurring approximately once every 10 years, and B and C serotypes are most common in the United States and Europe. Patients with inherited or acquired complement deficiency, HIV, and splenic dysfunction are at particular risk. Close living conditions (eg, due to low socioeconomic status, college dormitories, or military barracks) also represent a risk factor for rapid spread.
Meningococcemia often progresses rapidly to multisystem organ failure, due to activation and dysregulation of the coagulation cascade, leading to both microvascular thrombi and increased risk of bleeding. Disseminated infection can occur both with and without the presence of meningitis. The exact incidence of meningococcemia-associated acute adrenal insufficiency is unclear, given the lack of specific symptoms associated with this diagnosis and the frequent absence of the classic findings of necrosis or hemorrhage on early CT imaging. Classically, up to 75% of patients with meningococcemia and acute adrenal insufficiency have a skin rash, which typically rapidly transforms from small macules or papules into petechiae and progressive purpura. Ceftriaxone is the first-line treatment for N meningitidis in addition to supportive care for multisystem organ failure, and targeted transfusion therapy may be necessary when severe bleeding occurs. IV immunoglobulin may have a role in reducing toxin-mediated injury. While acute adrenal insufficiency was first described in N meningitidis infection, other bacterial and viral infections have subsequently been associated with this complication, including Streptococcus pneumoniae, Haemophilus influenzae, Escherichia coli, Staphylococcus aureus, Legionella pneumophilia, Bacillus anthracis, group A β-hemolytic Streptococcus and Capnocytophaga species, cytomegalovirus, and parvovirus B19.
Methylene blue has been used as a rescue therapy for patients with refractory septic shock; despite reducing the time to vasopressor discontinuation, it has had no impact on mortality in prospective randomized clinical trial data to date. While there is mounting evidence that patients who are critically ill are thiamine deficient and retrospective data have suggested IV supplementation may offer benefit in septic shock, the only prospective randomized clinical trial to date failed to demonstrate a reduction in acute kidney injury or mortality. Although retrospective studies suggested clinical benefit with the administration of vitamin C, hydrocortisone, and thiamine to patients in septic shock, several subsequent large prospective, placebo-controlled randomized trials have failed to demonstrate any benefit.1234567
A 24-year-old patient presents to the emergency department with 3 days of progressive diarrhea, abdominal pain, fever, headache, and rapidly deteriorating mental status. Medical history is significant for obesity complicated by type 2 diabetes mellitus, OSA, and hypertension. The patient is intubated for airway protection and treated with vancomycin and piperacillin-tazobactam. CT scans of head and abdomen are normal, and lumbar puncture is performed prior to ICU transfer for ongoing management.
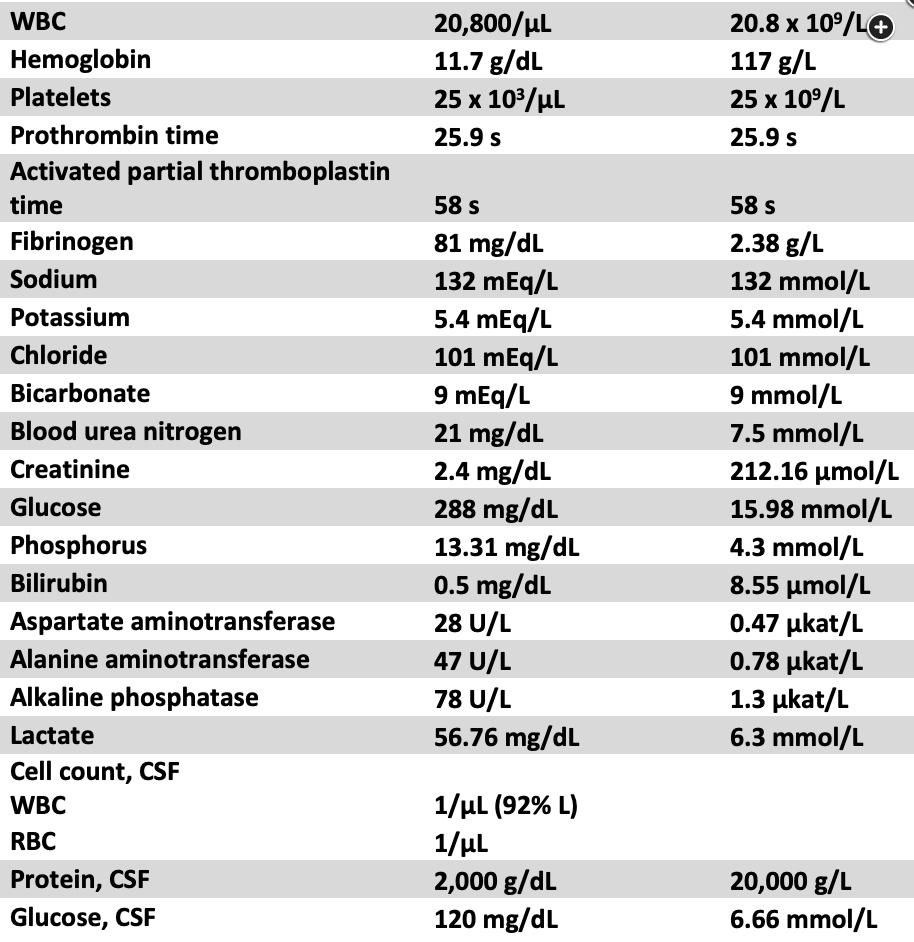
On ICU arrival, the patient is sedated and intubated. Temperature is 39.3 °C, heart rate is 135/min, BP is 105/65 mm Hg on 0.18 μg/kg/min norepinephrine and 0.04 U/min vasopressin, and SpO2 is 95% on volume-targeted assist-control ventilation. Physical examination is significant for nonfocal neurologic exam, tachycardia without obvious murmur, diminished bilateral breath sounds, and soft and nontender abdomen. There is blood in the mouth and diffuse rash with scattered petechiae and areas of confluent purpura (Figure 1 and Figure 2). Initial laboratory findings are summarized in Figure 3. Point-of-care ultrasound demonstrates hyperdynamic cardiac function without lung consolidation or free abdominal fluid. Vasopressor requirements continue to rapidly escalate during initial evaluation.
Which treatment is most appropriate to add at this time?
Links to this note
Footnotes
-
Ibarra-Estrada M, Kattan E, Aguilera-González P, et al. Early adjunctive methylene blue in patients with septic shock: a randomized controlled trial. Crit Care. 2023;27(1):110. PubMed ↩
-
Lyu QQ, Zheng RQ, Chen QH, et al. Early administration of hydrocortisone, vitamin C, and thiamine in adult patients with septic shock: a randomized controlled clinical trial. Crit Care. 2022;26(1):295. PubMed ↩
-
Moskowitz A, Berg KM, Grossestreuer AV, et al. Thiamine for Renal Protection in Septic Shock (TRPSS): a randomized, placebo-controlled, clinical trial. Am J Respir Crit Care Med. 2023;208(5):570-578. PubMed ↩
-
Sevransky JE, Rothman RE, Hager DN, et al; VICTAS Investigators. Effect of vitamin C, thiamine, and hydrocortisone on ventilatorand vasopressor-free days in patients with sepsis: the VICTAS randomized clinical trial. JAMA. 2021;325(8):742-750. PubMed ↩
-
Takada S, Fujiwara S, Inoue T, et al. Meningococcemia in adults: a review of the literature. Intern Med. 2016;55(6):567-572. PubMed ↩
-
Woolum JA, Abner EL, Kelly A, et al. Effect of thiamine administration on lactate clearance and mortality in patients with septic shock. Crit Care Med. 2018;46(11):1747-1752. PubMed ↩