opioid impact on sleep disordered breathing
- related: Sleep and Sleep Disordered Breathing
- tags: #literature #pulmonology
Both acute and chronic opioid use have a significant impact on sleep architecture and sleep-related respiratory disorders. Acute opiate use promotes stage 2 sleep and wake time after sleep onset, while decreasing slow wave sleep. With chronic use, sleep stage distributions may normalize, though withdrawal can be associated with a rebound increase in stage 3 and REM phase sleep.
Central sleep apnea is overwhelmingly the most common type of sleep-disordered breathing among opiate users, with the major risk factors being opiate dose and low-to-normal body weight (which presumably is associated with higher tissue levels of the drugs) (choice A is correct). Although OSA may worsen with opioids, presumably secondary to increased airways resistance due to relaxation of upper airway dilator muscles, in a randomized, cross-over trial, patients with OSA who received a one-time dose of 40 mg controlled-release oral morphine before sleep did not experience any worsening of OSA compared to placebo. Importantly, the prevalence of opioid-induced obstructive sleep apnea is far lower than that of opioid-induced central apnea (choice B is incorrect). All opiates are associated with the induction of central apnea, with the dose equivalent being a greater driver of the degree of disease induced than the specific opiate used (choice D is incorrect).
The specific constellation of polysomnographic findings in central sleep apnea due to opiate use is distinct from other types of central sleep apnea (choice C is incorrect). Two distinct respiratory patterns are strongly suggestive of opioid-induced central apnea: ataxic breathing and cluster breathing. Ataxic breathing (Figure 1) is associated with a high degree of variability in respiratory rate, tidal volume, and duration of central events; it is disorganized, and reliably lacks the crescendo-decrescendo pattern seen in Cheyne-Stokes breathing. Cluster breathing (Figure 2) is somewhat more regular appearing, typically characterized by a run of several deep breaths, accompanied by occasional intervening central apneas, which can be of variable length. Both of these findings tend to occur predominantly during non-REM sleep.
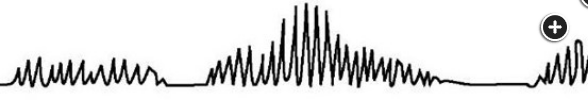
- ataxic breathing
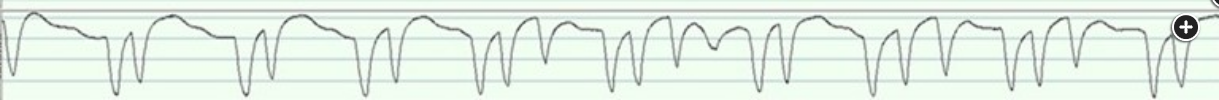
- clustered breathing1