order CPET to diagnose chronic dyspnea and assess preoperative risks
- related: cardiopulmonary exercise test CPET
- tags: #pulmonology #literature #pulmonology
Links to this note
During preoperative evaluation for lung resection, a cardiopulmonary exercise test (CPET) is recommended when the predicted postoperative (PPO) FEV1 or DLCO is less than 30% (choice B is correct).
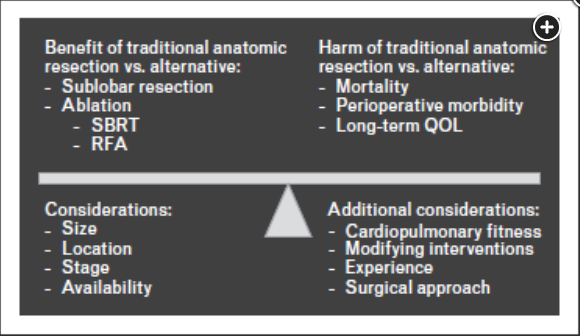
- Abbreviations: SBRT, stereotactic body radiation therapy; RFA, radiofrequency ablation; QOL, quality of life.
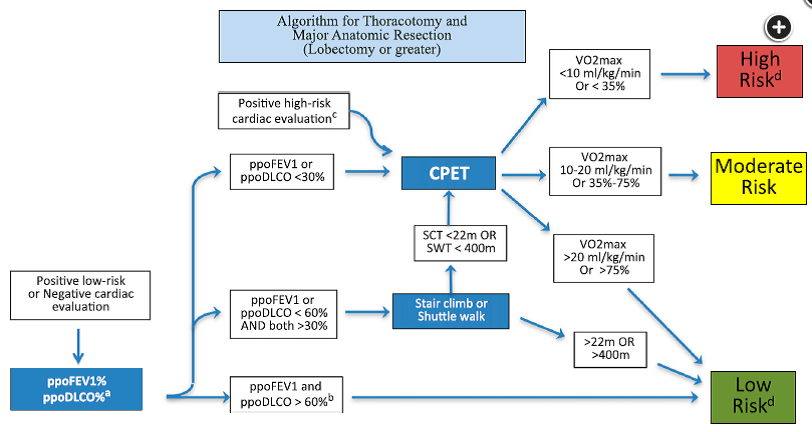
- Abbreviations: CPET, cardiopulmonary exercise testing; SWT, shuttle walk test; ppo, predicted postoperative. Figure courtesy of Brunelli A, Kim AW, Berger KI, Addrizzo-Harris DJ. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 suppl):e166S-e190S.
The choice of treatment for localized non-small cell lung cancer involves balancing the benefit and harms of a lobectomy or pneumonectomy with those of alternative treatment options while considering cancerand patient-related factors that may influence that balance (Figure 1). Lung resection remains the treatment of choice for individuals with early-stage lung cancer whose cardiopulmonary fitness is adequate to allow them to tolerate the extent of resection required with acceptable shortand long-term outcomes. The transition from thoracotomy to video-assisted (and robot-assisted) approaches to lung resection has led to fewer surgery-related complications while maintaining cancer outcomes. Improvement in our understanding of manifestations that allow for acceptable oncologic outcomes with sublobar resection (eg, subsolid lesions, solid cancers <2 cm in diameter with no cancer identified from complete lymph node sampling) has widened the cohort of individuals who could be considered fit for lung resection. Ablative therapies, particularly stereotactic body radiotherapy, have emerged as excellent alternatives to lung resection in individuals with stage I lung cancer who are considered high risk for lung resection. An expert panel identified the need for supplemental oxygen because of underlying lung disease, low diffusing capacity, frailty, and low functional status as indicators of high surgical risk.
The early and long-term risk of lung cancer resection is influenced by a patient's cardiopulmonary fitness. The Thoracic Revised Cardiac Risk Index can be used to identify patients at risk for cardiac complications. Those with any combination of the following conditions should undergo noninvasive cardiac stress testing or a cardiology consultation: previous ischemic heart disease, stroke or transient ischemic attack, creatinine level greater than 2 mg/dL (176.80 μmol/L), or planned pneumonectomy. Similarly, patients with a cardiac condition requiring medication or with a newly suspected cardiac condition and those unable to climb two flights of stairs should be considered for noninvasive cardiac stress testing or a cardiology consultation (choice A is incorrect). An echocardiogram may be considered to assess right ventricular function when a pneumonectomy is being considered. Right-sided heart catheterization is not recommended (choice C is incorrect).
Measurement of both the FEV1 and DLCO is recommended because both are predictive of postoperative morbidity and mortality. PPO estimates of postbronchodilator FEV1 and DLCO should be performed using either the segment method ((19 total segments − number of segments to be resected)/19) × preoperative FEV1 or DLCO % predicted) or the results of quantitative perfusion imaging (preoperative FEV1 or DLCO % predicted × (100 − % perfusion to the region to be resected/−100)). Both methods adequately estimate postoperative values for patients being evaluated for a lobectomy. In the patient in question, the PPO DLCO was 38.4 × (14/19) = 28.3%.
e.g.
Pulmonary function testing reveals a postbronchodilator FEV1 of 2.12 L (78.2% predicted) and DLCO of 15.7 mL/min/mm Hg (69.5% predicted). Quantitative perfusion imaging showed 49% perfusion to the right lung, with 5% to the right upper and 44% to the right lower zones.
With the information provided in the question, this patient would have a predicted postoperative (ppo)FEV1 of 39.9% predicted and a ppoDLCO of 35.4%. If either the ppoFEV1 or ppoDLCO is between 30% and 60% predicted, an exercise test is recommended to stratify the risk of pulmonary complications further (Figure 2) (choice D is correct).
Patients with a PPO FEV1 and PPO DLCO greater than 60% predicted are considered low risk for resection. Patients at moderate risk for surgical complications on the basis of pulmonary function testing include those with PPO FEV1 or PPO DLCO 30% to 60% predicted. Guidelines recommend that this group undergo exercise testing with low-technology tests such as the shuttle walk test (SWT), stair climbing test (SCT), or 6-min walk test (6MWT) to assist further with risk prediction. Those with impaired performance on these tests (SWT distance <1,333.33 ft [400 m]; SCT height <73.33 ft [22 m]; 6MWT <1,000 ft [300 m], desaturation ≥4%, or heart rate recovery ≤12), or those at high risk on the basis of pulmonary function measures (PPO FEV1 or PPO DLCO <30%), should undergo further evaluation with a formal CPET (choice D is incorrect). Those with a peak oxygen consumption (VO2peak) greater than 20 mL/kg/min or greater than 75% predicted are considered low risk for resection; those with a VO2peak of 10 to 20 mL/kg/min or 35% to 75% predicted are considered moderate risk for lung resection; and those with a VO2peak less than 10 mL/kg/min or less than 35% predicted are considered high risk for lung resection. A more sophisticated interpretation of the results of the CPET (eg, cardiac or ventilatory limitation, ventilation reserve) can assist with risk prediction for the sizable number of patients who are within the moderate risk range (Figure 2).
Shortand long-term harms from surgical resection related to cardiopulmonary fitness may be modified by optimizing treatment of comorbid conditions (eg, COPD), smoking cessation, and optimization of fitness (eg, pulmonary rehabilitation).3
Footnotes
-
Colice GL, Shafazand S, Griffin JP, Keenan R, Bolliger CT; American College of Chest Physicians. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: ACCP evidenced-based clinical practice guidelines (2nd edition). Chest. 2007 Sep;132(3 Suppl):161S-77S. doi: 10.1378/chest.07-1359. PMID: 17873167. ↩