oxygen therapy improves survival in patients with resting hypoxemia
- related: COPD chronic obstructive pulmonary disease
- tags: #literature #pulmonology
The current indications for long-term oxygen therapy (LTOT) remain largely based upon two nonblinded, randomized controlled trials performed in the 1970s. These established that LTOT given for ≥15 h/d improved survival vs nocturnal-only oxygen use or no oxygen therapy. Participants had COPD and chronic severe hypoxemia with a resting Pao2 of ≤55 mm Hg (or Spo2 of ≤88%), or they had Pao2 of 56 to 59 mm Hg (or Spo2 of 88% to 90%) with evidence of cor pulmonale or polycythemia. Only the woman with a resting Spo2 of 89% and P pulmonale on ECG meets these criteria.
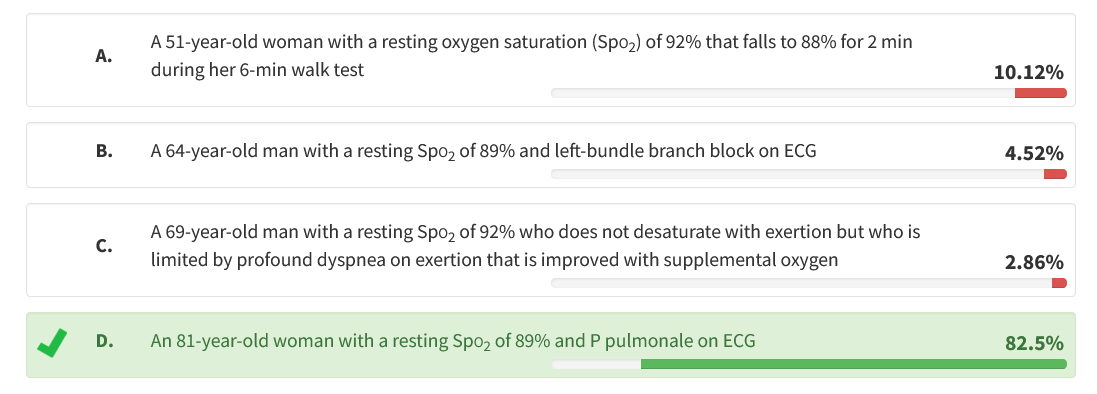
In 2016, the benefit of LTOT in patients with COPD and less severe hypoxemia was examined. A randomized trial of 738 patients in 42 centers enrolled patients with stable COPD and Spo2 of 89% to 93% at rest and/or with exercise-induced desaturation during the 6-min walk test to Spo2 of <90% for >10 s but also remaining at ≥80% for ≥5 min of the 6-min test. LTOT in these patients did not result in a longer time to death or first hospitalization vs no long-term supplemental oxygen, nor did it provide sustained benefit with regard to measures of quality of life, lung function, and the distance walked in 6 min. Note that in the 64-year-old man with a resting Spo2 of 89%, the ECG finding of a left-bundle branch block is not evidence of cor pulmonale.
In some cases, supplemental oxygen provides symptomatic dyspnea relief by stimulating a decrease in minute ventilation, and may improve activity. However, reported symptomatic benefit with oxygen in the absence of the listed accepted criteria has not been demonstrated to improve survival. Dyspnea on exertion in patients with COPD has a differential diagnosis beyond exertional hypoxemia, including mechanical loading of the respiratory system, deconditioning, and concomitant cardiac disease. Pulmonary rehabilitation can result in meaningful improvements in dyspnea despite minimal impacts on pulmonary function or oxygenation.1