PEEP and plateau in APRV
- related: basic understanding of ventilators
- tags: #literature #pulmonary
Links to this note
APRV is a mode that is based on machine/patient-triggered, pressure-targeted, and time-cycled breaths that is set in a prolonged inspiratory time/short expiratory time configuration (inverse ratio ventilation). It is similar in concept to older inverse ratio strategies but differs in that spontaneous breaths are allowed. In theory, inverse ratio strategies offer the advantage of mean airway pressure elevations and consequent alveolar recruitment without having to add PEEP or tidal volume. Outcome studies, however, are limited and conflicting.
An underappreciated aspect of APRV is that the short expiratory time often recommended by those experienced with using APRV results in the buildup of significant auto-PEEP. In this patient, auto-PEEP should be expected, since the expiratory flow does not return to zero during the short expiratory time (Figure 2, yellow arrow). Indeed, an expiratory pause maneuver demonstrates a total of 12.8 cm H2O auto-PEEP above the set PEEP of 0 cm H2O (Figure 3, yellow arrow). At the same time, the set Phigh of 20 cm H2O is identical to the end-inspiratory Pplat in the lungs. Importantly, the calculated driving pressure (Pplat − PEEP) using the applied PEEP (0 cm H2O) yields an excessive value of 20 cm H2O. However, when using the correct PEEP level, driving pressure is in a relatively safe range (ie, 20 − 12.8 = 7.2 cm H2O).
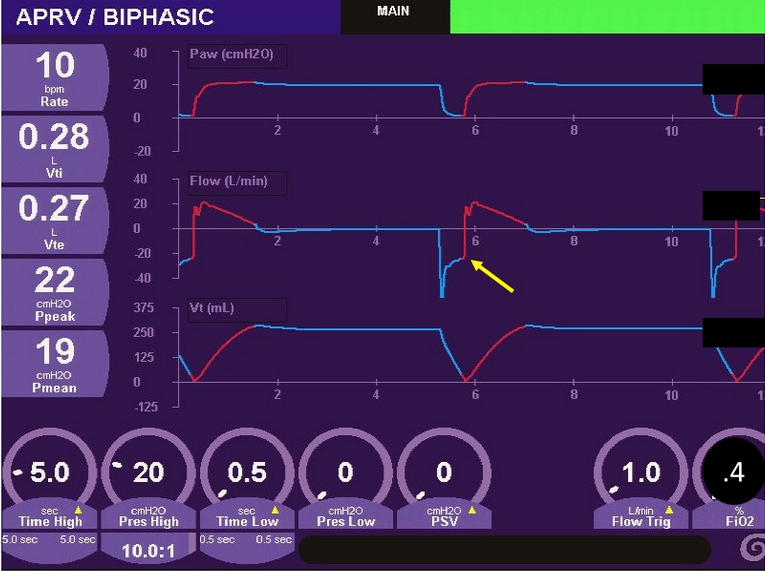
- Airway pressure, flow, and volume over time from a patient on APRV. Yellow arrow indicates incomplete exhalation suggesting the presence of auto-PEEP.
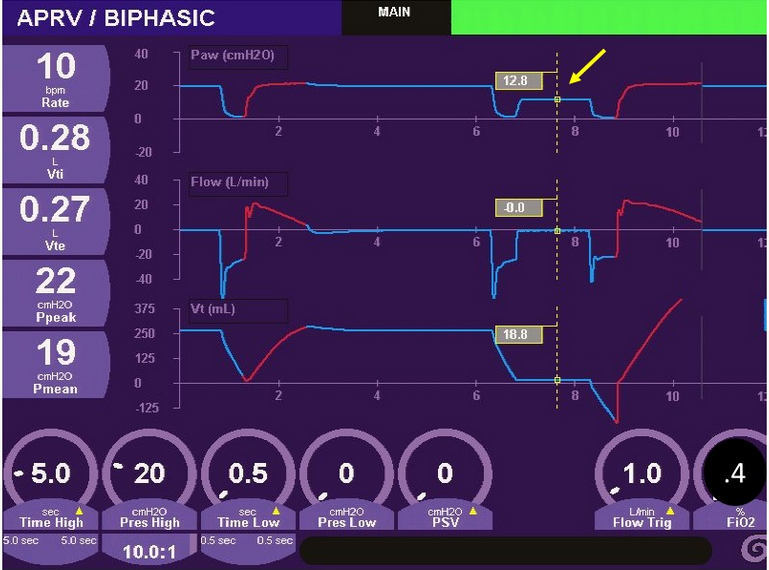
- Airway pressure, flow, and volume over time from a patient receiving APRV. Yellow arrow indicates a measured auto-PEEP of 12.8 cm H2O obtained from an expiratory pause maneuver.
It is important to remember that auto-PEEP and applied PEEP distribute differently and may have different recruitment effects. Applied PEEP distributes equally throughout the lungs to all units with patent airways. In contrast, auto-PEEP develops predominantly in units with slow expiratory time constants (ie, high-resistance, high-compliance units) that may not be optimal in parenchymal lung injury.
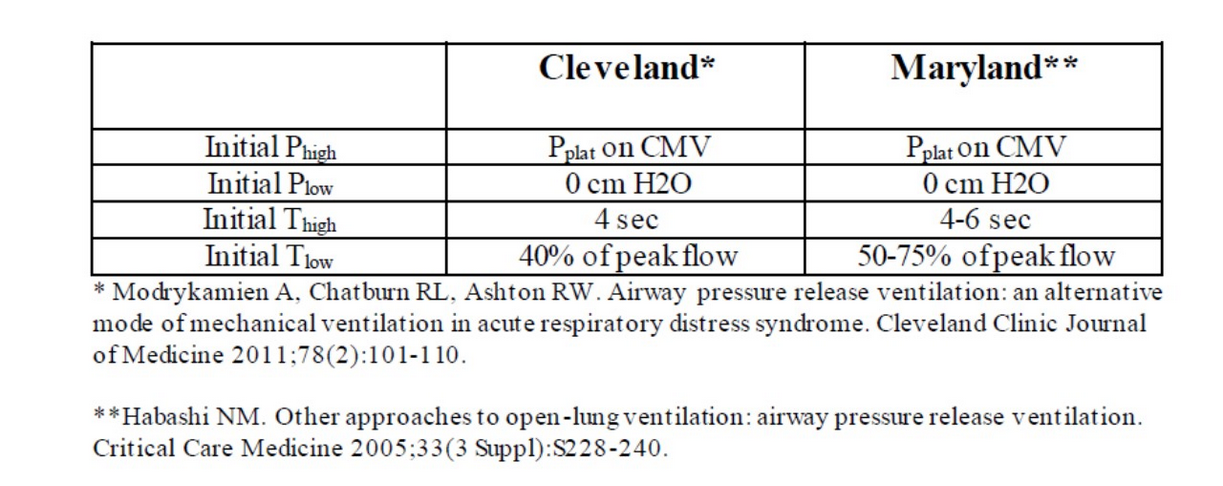
Consensus about proper APRV settings does not exist. Figure 4 summarizes recommendations from two groups with considerable APRV experience. An additional feature to APRV that clinicians need to appreciate is that spontaneous breaths, with or without pressure support, are allowed (even encouraged) during the inflation from Phigh. When these are present (not in this patient), the patient-generated negative pressure can add to the Phigh to increase end-inspiratory transpulmonary pressure to potentially dangerous levels.1