pulmonary artery catheter dos and donts
- related: pulmonary artery catheter
- tags: #literature #icu
The PAC, also known as the Swan-Ganz catheter, is a balloon-flotation vascular catheter designed to be inserted via a major vein and advanced through the right heart with placement of the tip of the catheter into a pulmonary artery (PA). The catheter is used to display intravascular pressures within the right atrium (RA), right ventricle (RV), and PA as the catheter tip is advanced into a PA occlusion or wedge position.
While generally safe, there are multiple opportunities for complications during PAC insertion and maintenance and thus important caveats to consider for safe PAC use. Of the statements listed, “Inflate the balloon at the tip of the PAC with air gradually while monitoring the waveform” is accurate, while the others are incorrect. Placement of the catheter into proper position is dependent upon inflation of a small balloon (1.5-mL capacity) near the tip of the catheter with air, which serves as a sail, helping to propel the catheter tip along with the flow of blood. Continuous display of pressure waveforms allows ongoing monitoring of the position of the catheter tip during insertion and after placement. The balloon also serves to occlude a PA branch, thus allowing display and measurement of the PA occlusion pressure (PAOP), also called the pulmonary capillary wedge pressure or wedge pressure. Under many clinical circumstances, PAOP is a reasonable surrogate for left atrial pressure and left ventricular end-diastolic pressure as the pressure waves are propagated retrograde through the pulmonary veins and capillaries to the balloon-occluded PA. Demonstrating transition from a PA waveform to a PAOP waveform during insertion or with balloon inflation, and return to a PA waveform during balloon deflation, confirms successful PAC placement. The characteristic waveforms seen during PAC insertion are displayed in Figure 1.
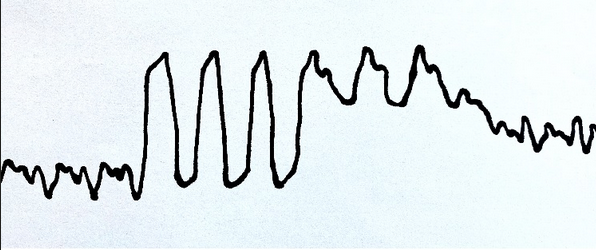
Depiction of waveforms as PAC is advanced through the right atrium (beats 1-3), right ventricle (4-6), pulmonary artery (7-9), transition to pulmonary artery occlusion or wedge (10), and pulmonary artery occlusion or wedge (11 and 12).
Proper inflation of the balloon is important. It should be inflated with air and not liquid. The wall tension of the balloon promotes rapid deflation when the inflating syringe is removed. Actively evacuating the air from the balloon with the syringe can rupture the balloon and should be avoided. Balloon inflation that is slow and accompanied by close observation of the waveform permits timely recognition that the catheter tip is within a small PA that might be ruptured with continued inflation. PA rupture is a potentially life-threatening complication. Transition from a PA to a PAOP waveform after injection of <1 mL of air into the balloon indicates that the catheter tip is probably in a small PA and the catheter should be retracted until this is corrected. This scenario is particularly common after the PAC has been in place for a while, since the catheter material softens and the catheter tip migrates further distally into a smaller vessel. A distal position of the PAC tip can often be detected on a chest radiograph.
There are additional important caveats to consider for safe PAC insertion. During preparation for insertion of a PAC, it is important to review the ECG for evidence of a preexisting left bundle branch block, since the catheter can provoke a right bundle branch block (RBBB) when it is within the RV, potentially producing complete heart block. However, preexisting RBBB will not place the patient at risk for this complication. Passage of the catheter tip through the RV commonly triggers premature ventricular contractions that can be sustained as ventricular tachycardia. Accordingly, rapidly advancing the catheter tip through the RV into the PA is preferred. If RV pressure measurements are sought, the RV waveform can be recorded during the rapid catheter tip transit through the RV for subsequent measurement after the procedure. During PAC insertion, difficulty may be encountered in achieving a satisfactory position within the PA, particularly if pulmonary hypertension is present. Accordingly, the PAC may need to be retracted back to a position within the vena cava or RA for another attempt at insertion. The balloon should be deflated for catheter retraction because it is possible to produce injury to the tricuspid valve as an inflated balloon encounters the valve and chordae tendineae during retraction. While the use of PACs has decreased in the past several decades, it continues to have utility in cardiovascular critical care. In addition to continuous display and measurement of intravascular pressures as described, the PAC can be used to measure cardiac output by thermodilution and supports the capability to sample blood from various sites to determine location of shunt. The ease of repeated measurements can be used to monitor response to hemodynamic manipulation.123456
Links to this note
Footnotes
-
Depiction of waveforms as PAC is advanced through the right atrium (beats 1-3), right ventricle (4-6), pulmonary artery (7-9), transition to pulmonary artery occlusion or wedge (10), and pulmonary artery occlusion or wedge (11 and 12). ↩
-
Bootsma IT, Boerma EC, de Lange F, et al. The contemporary pulmonary artery catheter. Part 1: placement and waveform analysis. J Clin Monit Comput. 2022;36(1):5-15. PubMed ↩
-
Bootsma IT, Boerma EC, Scheeren TWL, et al. The contemporary pulmonary artery catheter. Part 2: measurements, limitations, and clinical applications. J Clin Monit Comput. 2022;36(1):17-31. PubMed ↩
-
Lee M, Curley GF, Mustard M, et al. The Swan-Ganz catheter remains a critically important component of monitoring in cardiovascular critical care. Can J Cardiol. 2017;33(1):142-147. PubMed ↩
-
Magder S. Invasive hemodynamic monitoring. Crit Care Clin. 2015;31(1):67-87. PubMed ↩