pulmonary benign metastasizing leiomyoma PBML
- related: Pulmonary Diseases
- tags: #literature #pulmonology
Source
The imaging and the histopathology findings are consistent with the diagnosis of PBML. Benign metastasizing leiomyoma (BML) is a rare disorder that affects women with a history of uterine leiomyoma, occurring in all age groups, mostly between age 30 and 74, and is particularly prevalent among women of late childbearing age. Many women with BML diagnosed have a history of uterine leiomyoma or may have undergone leiomyoma resection or hysterectomy. Its clinical course is closely associated with sex hormone levels. The disease develops as a proliferation of multiple nodules composed of smooth muscle cells. BML is often associated with distant metastases as evidenced by proliferation of smooth muscle to the lungs, lymph nodes, abdomen, bone, spine, heart, mediastinum, nervous system, skin, and retroperitoneum. The lungs are the most common site of metastasis. Patients with PBML are often asymptomatic, though insidious onset of cough and dyspnea has been reported along with pneumothoraces, hemothoraces, and hemoptysis.
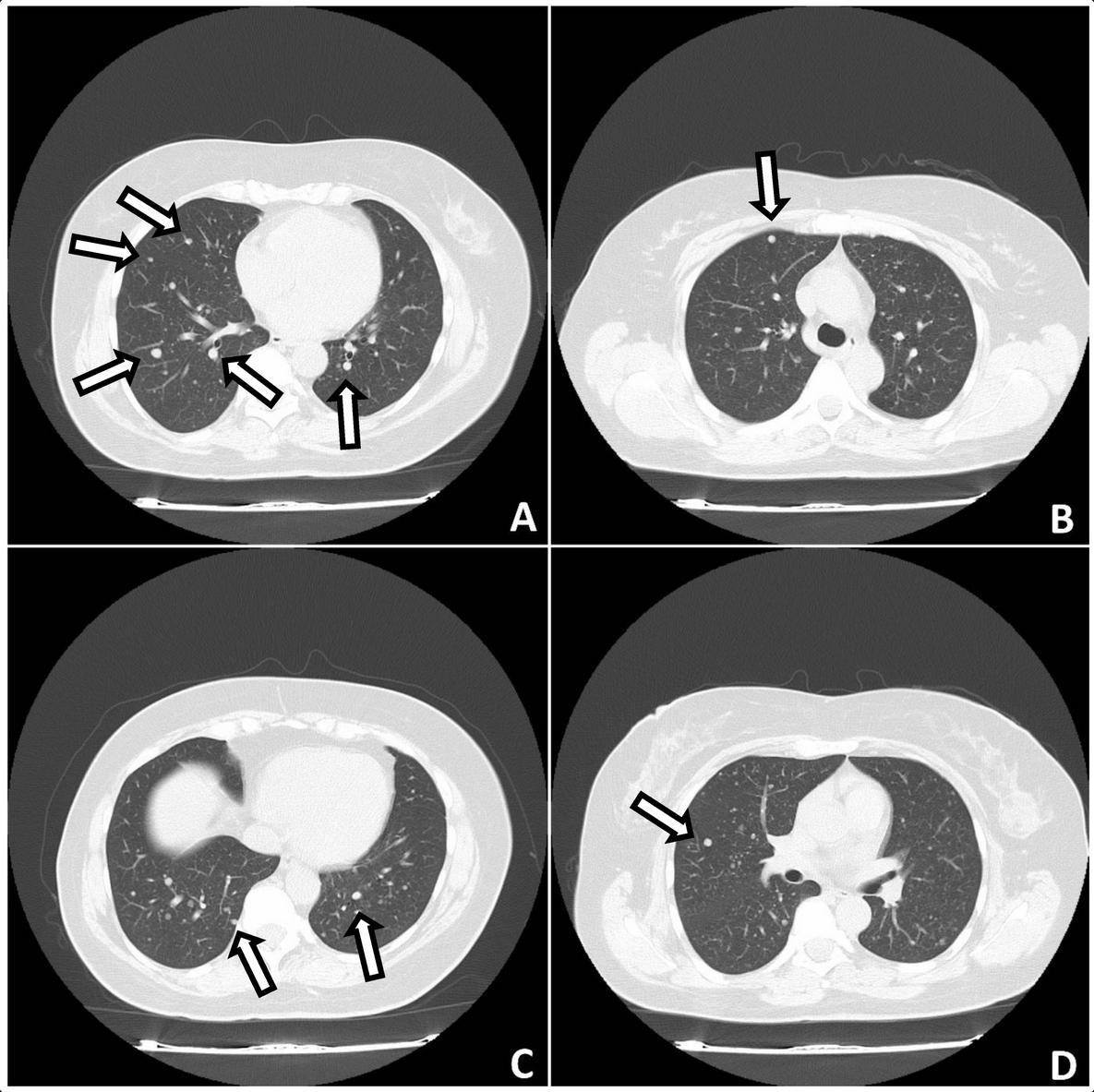
Typical radiographic findings include numerous random, well-circumscribed nodules that can occasionally display a miliary pattern, although solitary nodules can occasionally be seen. The nodules are mostly solid with no calcification but often cavitate; the edges are smoother and clearer without enhancement than those of malignant metastasis but may also be lobulated and display enhancement on contrast-enhanced CT scanning. On fludeoxyglucose F 18 PET, most pulmonary nodules of PBML show low or no metabolic activity, a feature that can occasionally be used to differentiate them from malignant metastasis.
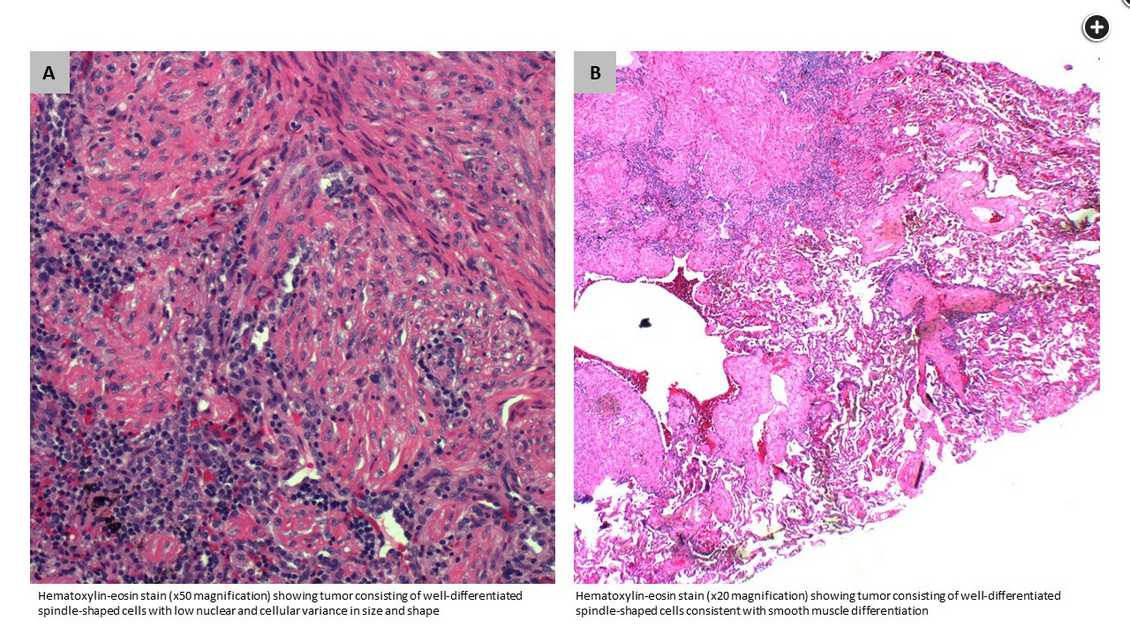
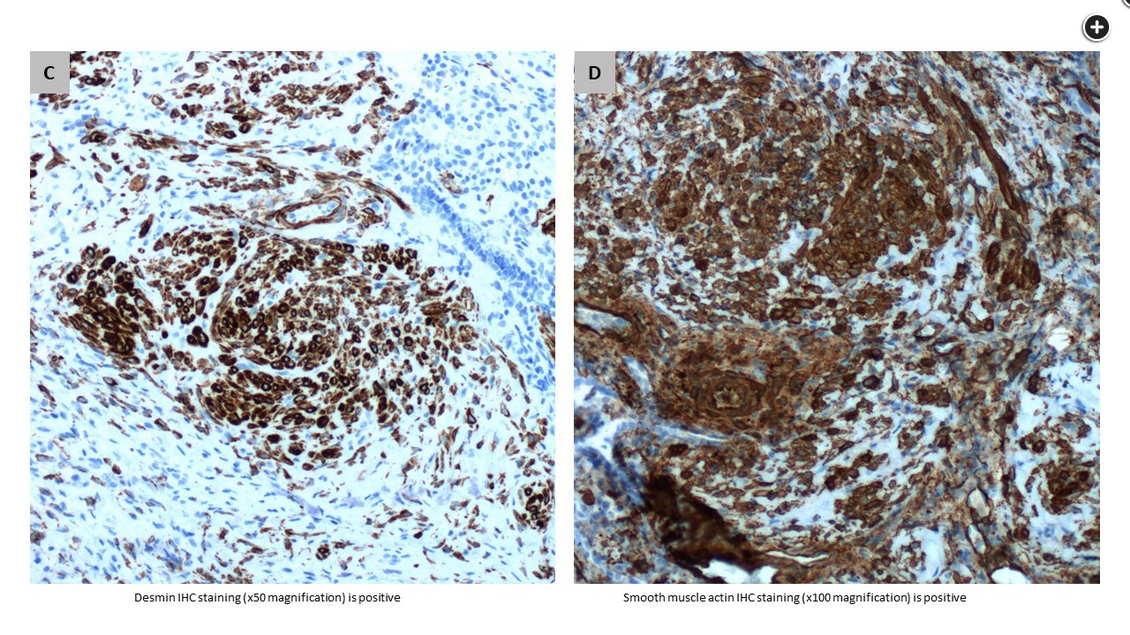
The diagnosis of PBML can be confirmed only through histopathological analysis. Histological evaluation shows uterine well-differentiated spindle-shaped cells with low nuclear and cellular variance in size and shape (Figure 3 and Figure 5). Additionally, immunohistochemical (IHC) staining for desmin, actin, caldesmon, and vimentin are often diffusely positive (Figure 4). A low mitotic index of fewer than five mitoses per 10 in a high-powered field, as also assessed by the Ki67 index, and the absence of necrosis suggest the benign nature of these tumors. These tumors are also diffusely and strongly positive for estrogen and progesterone receptors and negative for HMB-45.