pulmonary hypertension 1 31 2023 lecture
- related: Pulmonary Diseases
- tags: #literature
- source:
- 1035531
- usually presenting with exertional dyspnea
- edema, JVD
- RVH, RBBB, RV straining
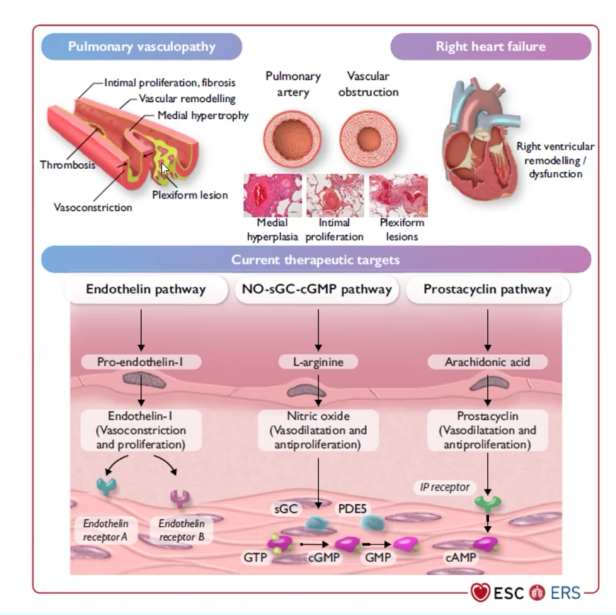
- PVOD
- echo can look for shunt
- PFT: isolated low DLCO
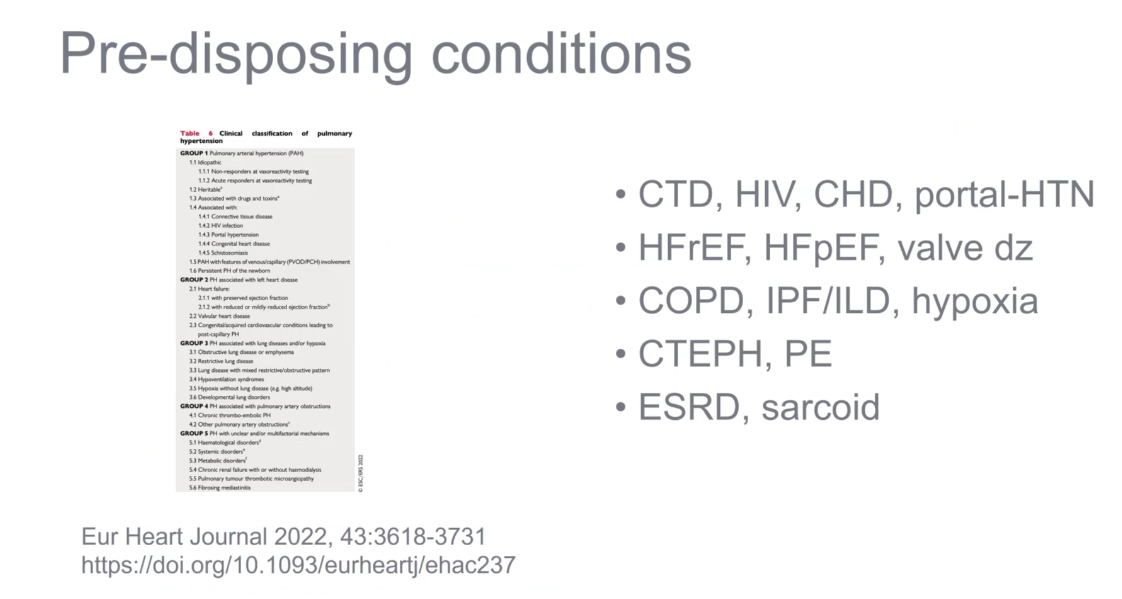
- ESRD and CKD can also cause PHTN.
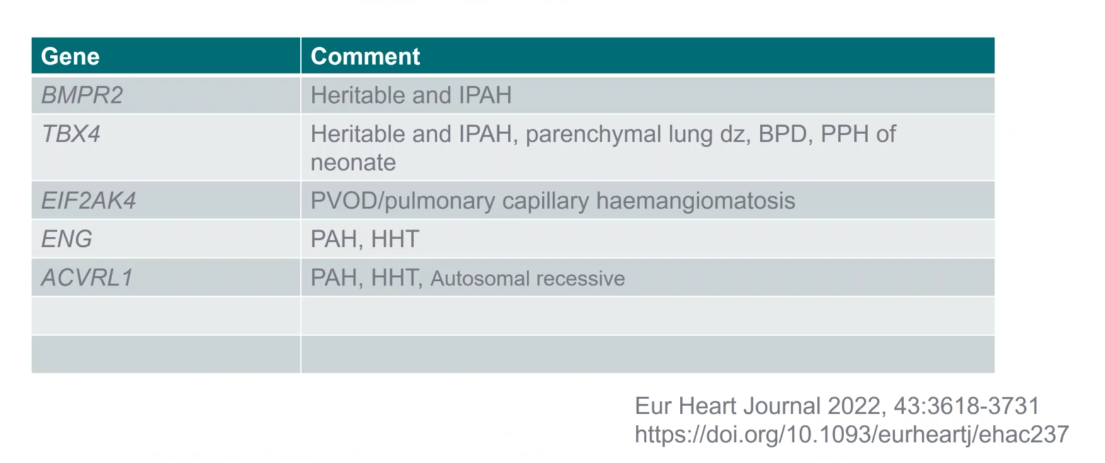
- HHT are at high risk for PHTN
- pulmonary capillary hemangiomatosis: can have worse outcome on vasodilators
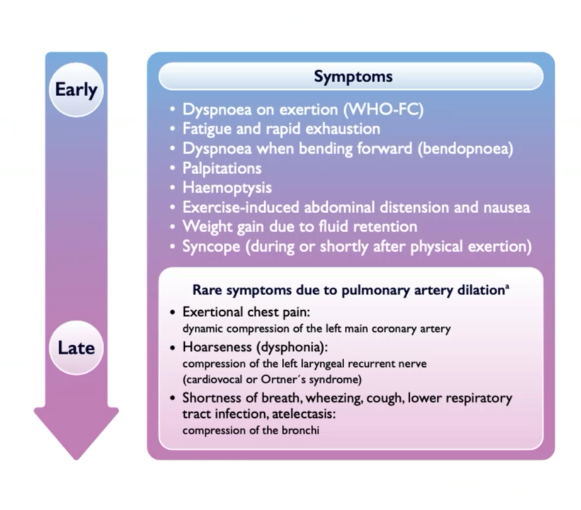
Symptoms and signs
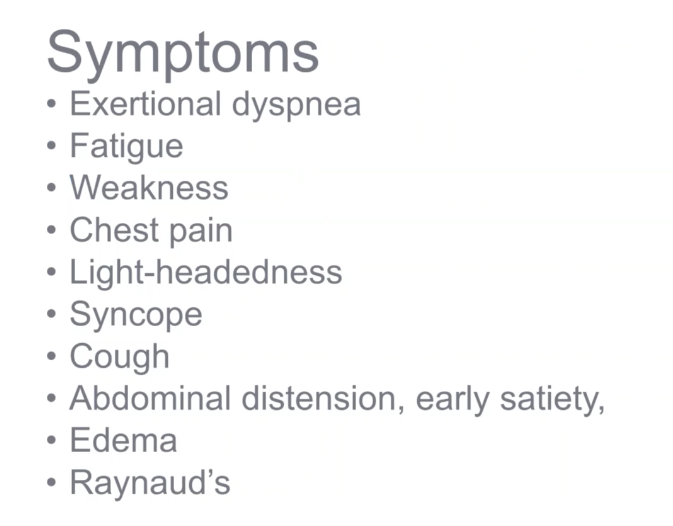
- mostly exertional dyspnea, goes back months
- low CO: weakness, fatigue, syncope
- dilated PA can compress left main coronary: chest pain
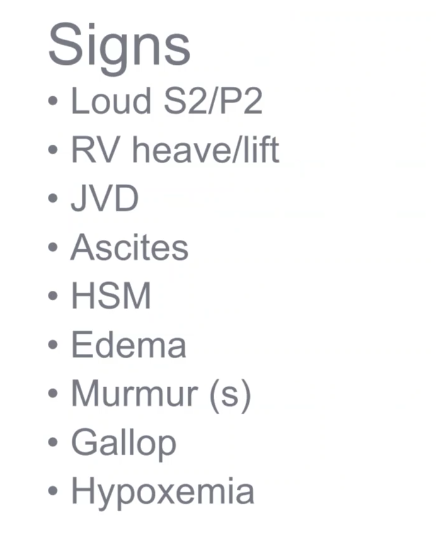
- 2nd heart sound should be loudest at base, but if loud at apex just as loud as first heart sound, it’s abnormal
Labs
- connective tissue panels not necessary unless they have physical findings
- muscle weakness
- rash
- joints
- skin changes
- thyroid problems
EKG
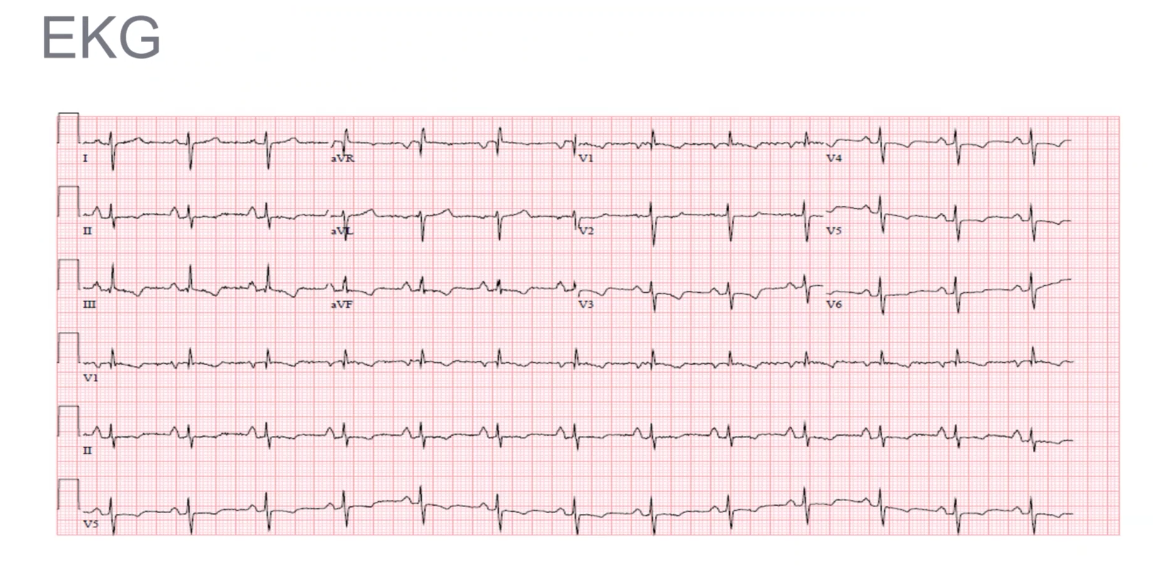
- presence of qR complex in V1 and RVH (tall R in V2 and S in V5)
- p wave > 25mm in II, p pulmonone
- ST depression, T wave inversion in inferior and anterior leads
Echo
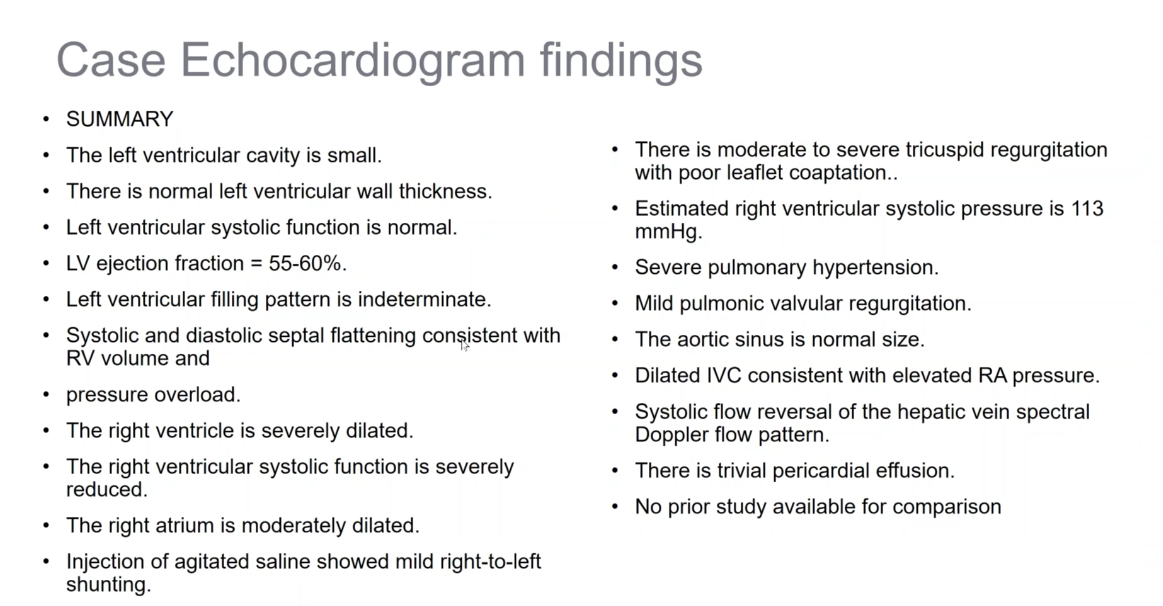
-
RV dysfunction can impair LV filling, usually indeterminate
-
pericardial effusion poor prognosis
-
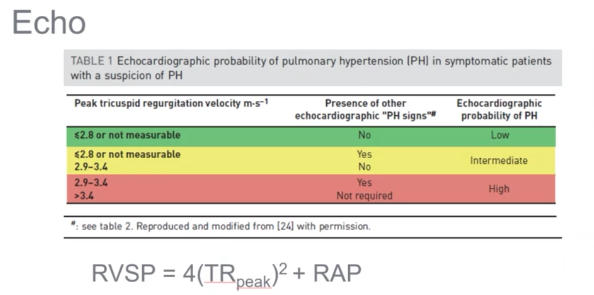
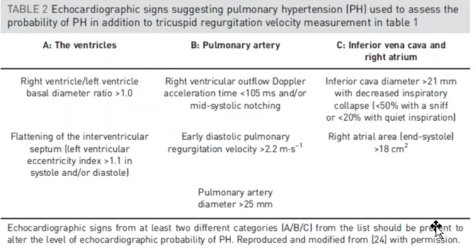
stop using RVSP as cut off
-
use TR jet as better measurement
-
Increasing suspicion based on velocity
-
TR > 3.4 m/s, confirms PHTN. RHC then only tells which type.
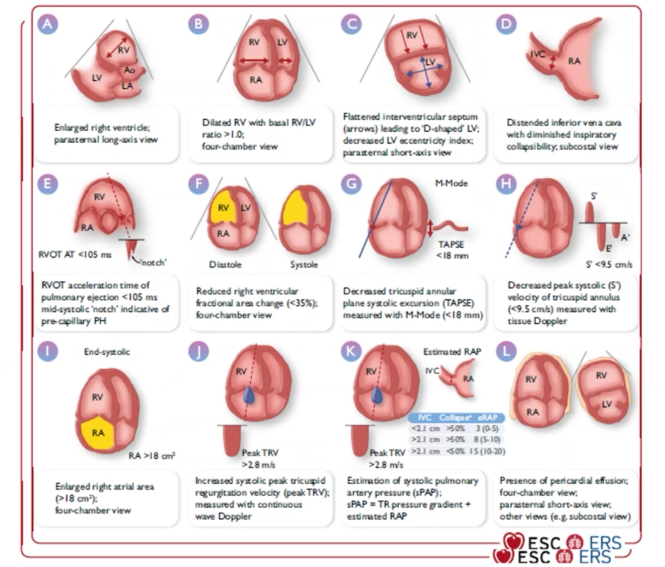
-
TAPSE: how RV adapting to high pressure. Lower TAPSE = higher mortality
CT
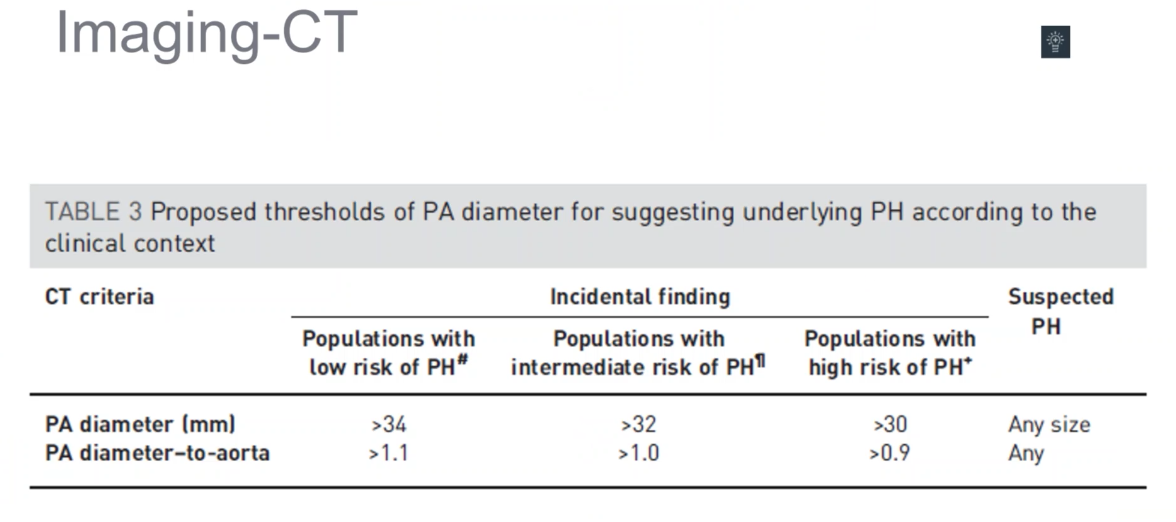
- index PA diameter to size of aorta
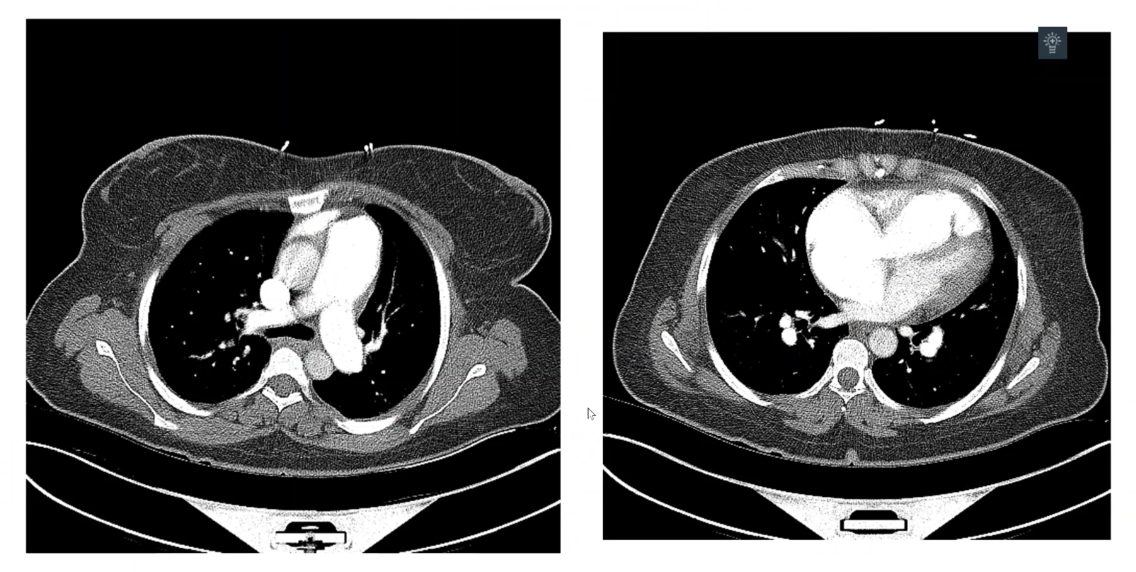
- dilated pulmonary arteries more distally
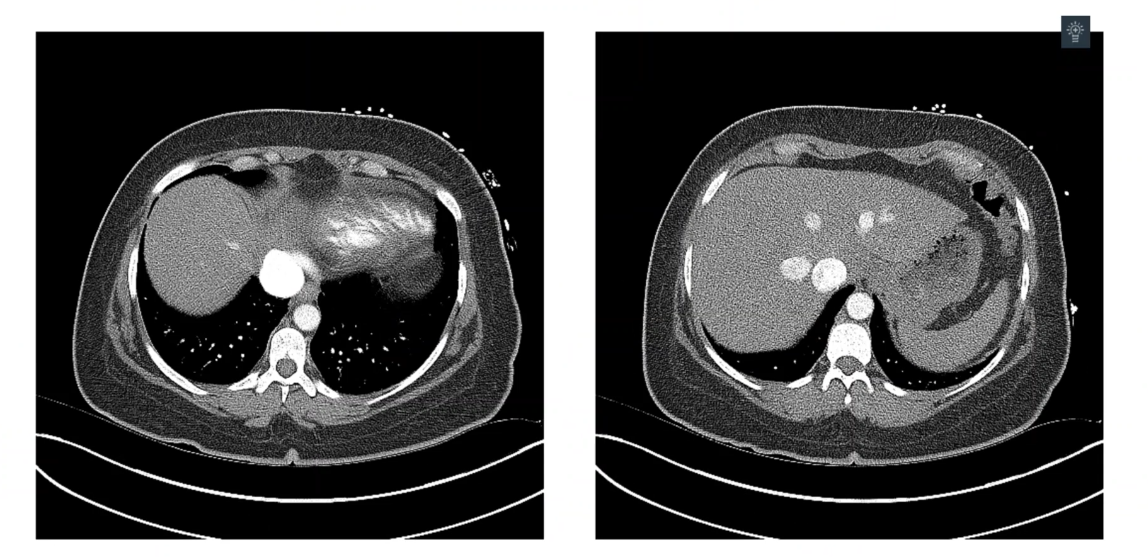
- dilated IVC
- regurgitated contrast
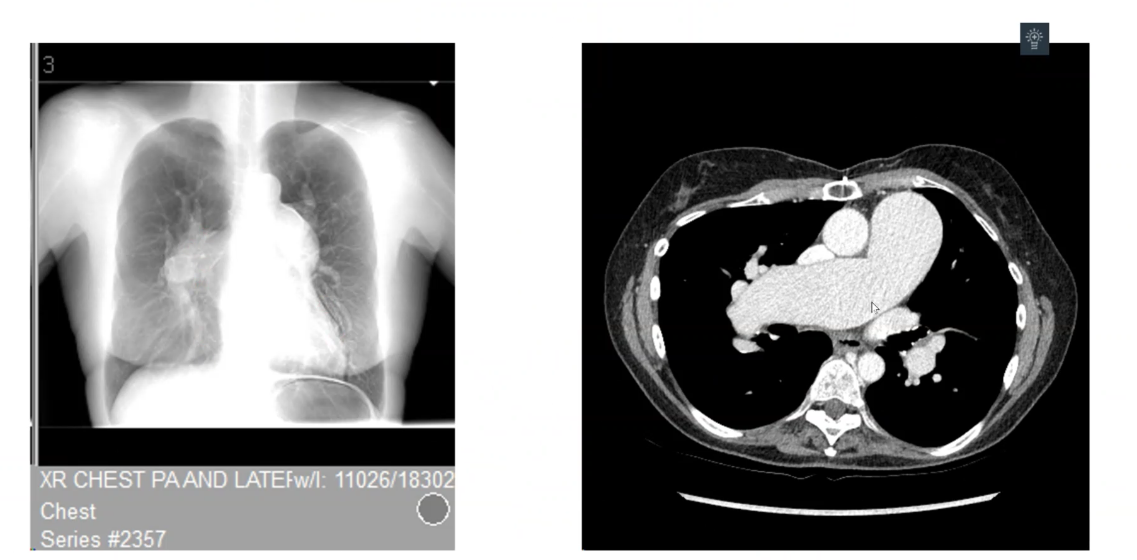
- PA dilation on CXR
Pathophysiology
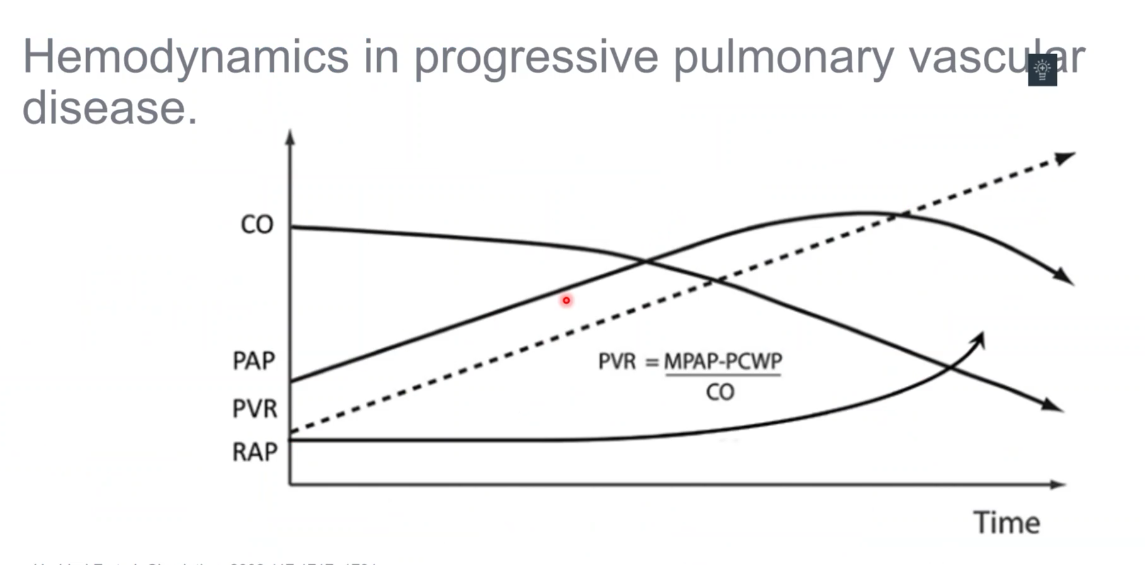
- after PVR gets to certain point, PAP goes down
- RAP and CO more important
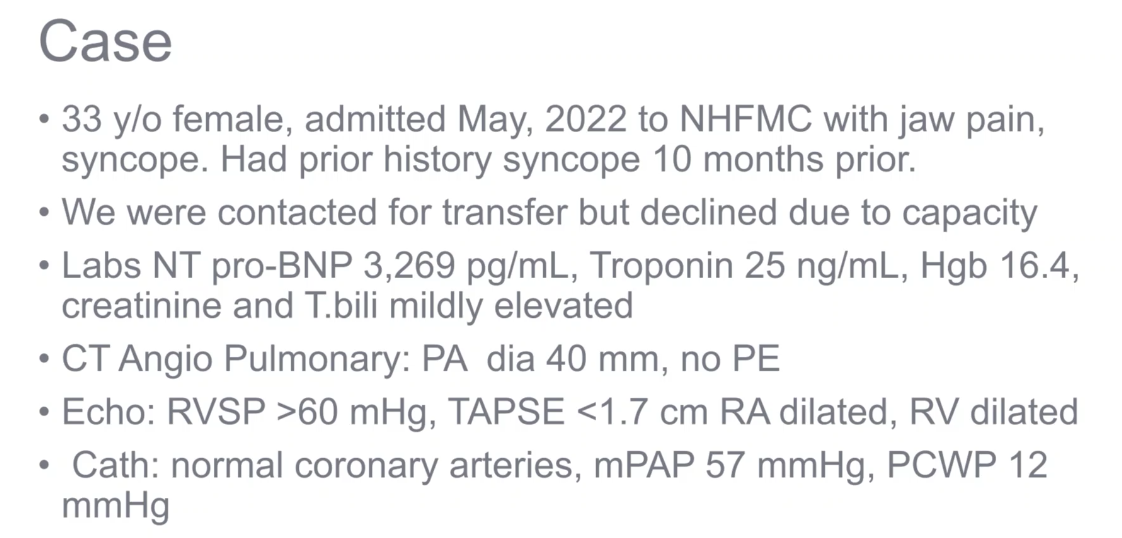
Case
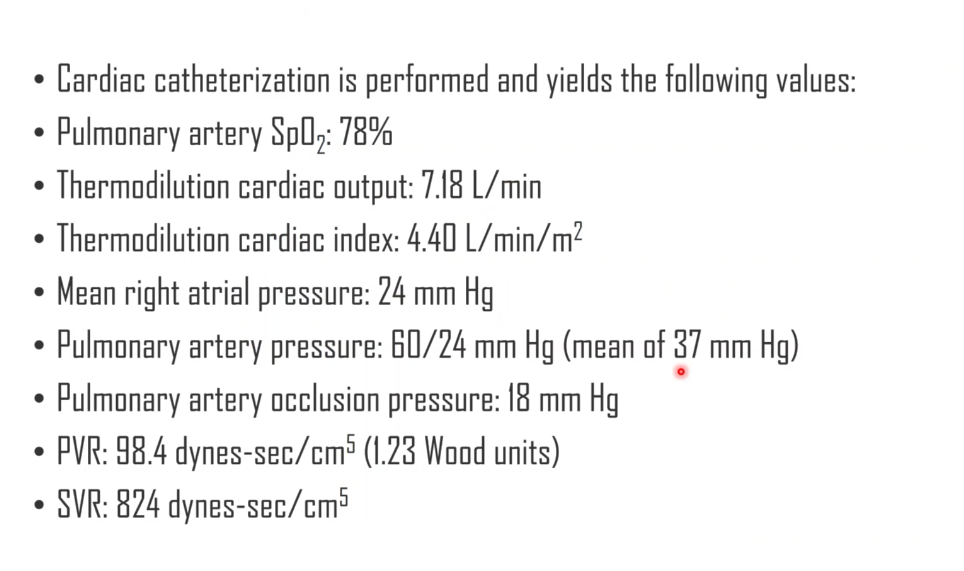
- hepatic AVM: L to R shunt
- hepatopulmonary syndrome: R to L shunt
- high output cardiac failure causing PHTN due to AVMS with HHS.
- ESRD patients with AV fistula could have similar problem
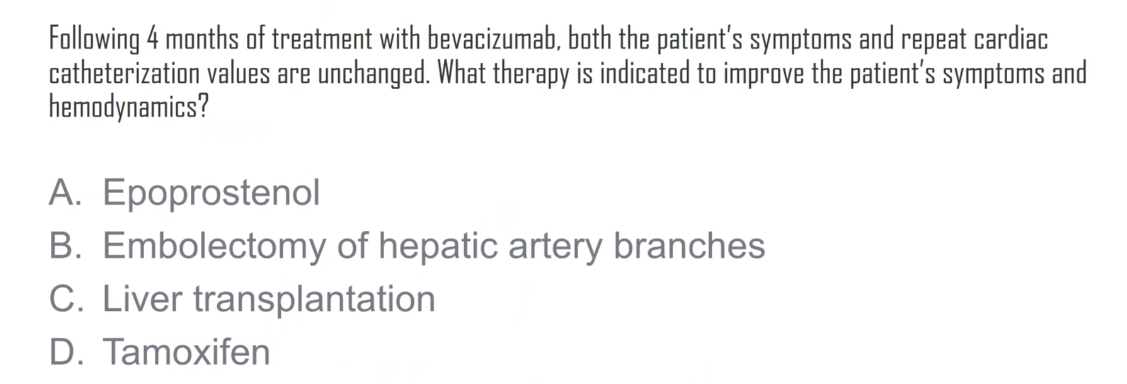
- A: vasodilate can cause worsening hypotension
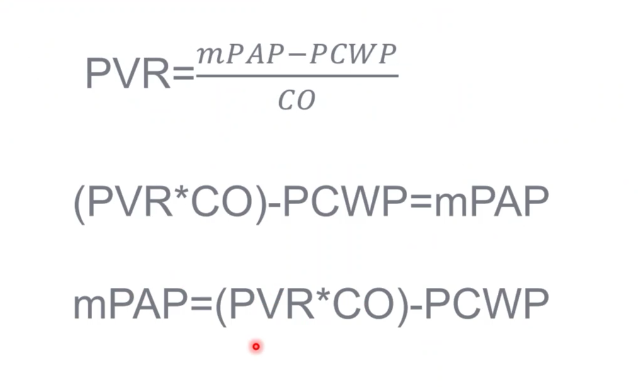
- PA pressure can go up with either increased CO or PVR
- high PCWP can actually be beneficial
Treatment
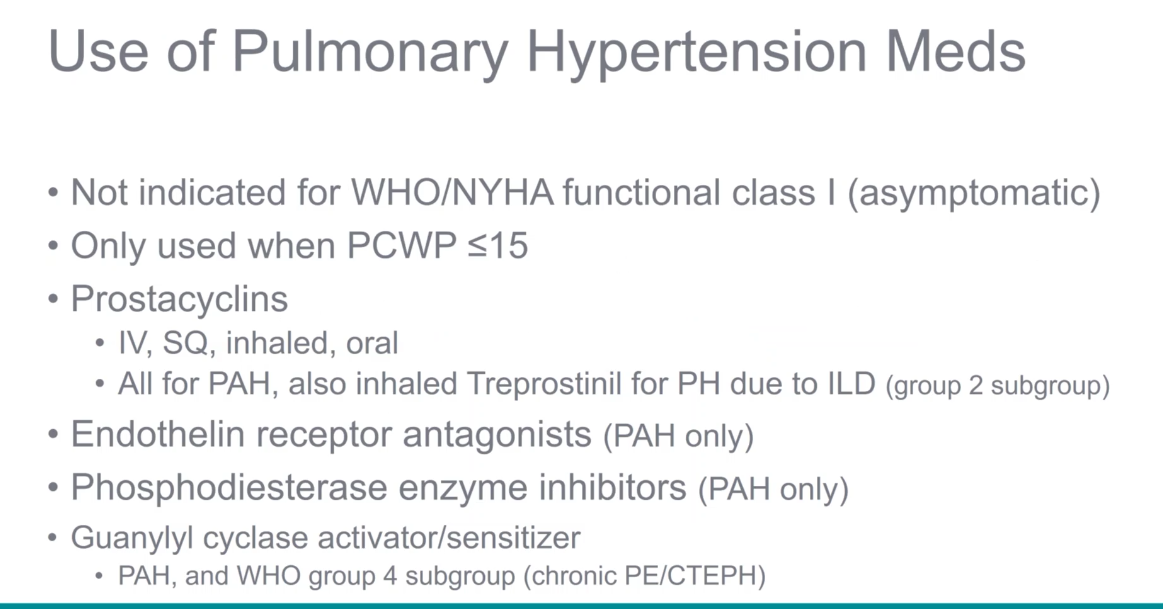
- oral drugs not great because of GI side effects