pulmonary vein thrombosis following lung transplant
- related: lung transplant and complications
- tags: #literature #icu
Pulmonary vascular anastomotic complications after lung transplantation, which includes pulmonary artery stenosis, kinking of the pulmonary artery, and pulmonary vein thrombosis (PVT), are associated with significant morbidity and mortality and occur in 1.8% to 5.2% of lung transplant recipients.
PVT is an early postoperative complication that occurs at the site of the pulmonary vein and/or left atrial anastomotic suture line. In a prospective study of 87 consecutive lung transplant recipients who underwent transesophageal echocardiography (TEE) within 48 h of the transplantation, 15% had pulmonary vein or left atrial thrombus, and the presence of thrombus was associated with a 90-day mortality of nearly 40%.
Complications from pulmonary vein anastomotic thrombosis may be catastrophic and include obstruction of pulmonary venous outflow, which results in severe pulmonary edema and hypoxemic respiratory failure that is refractory to medical management, early postoperative allograft failure, and systemic embolization of the thrombus with resultant stroke, as was seen in this patient.
Patients with PVT are often hypoxemic, with decreased lung compliance and diffuse infiltrates in the lung allograft. They may also have elevated pulmonary artery and central venous pressures. The diagnosis is most often made by TEE, which should be performed early in the evaluation of a lung transplant recipient with hypoxemic respiratory failure. Management is not uniform across transplant centers and is often dictated by the severity as assessed by TEE and clinical manifestations of the PVT. For small nonobstructive thrombus, a conservative approach may be advised. In symptomatic patients with medium or large thrombi, systemic anticoagulation or fibrinolytic therapy may be indicated; however, one must weigh the risk of bleeding in the early postoperative period against the potential benefit.
In patients with large, obstructive thrombi that manifest with hypoxemic respiratory failure or hemodynamic instability, emergent surgical thrombectomy has been reported, often with poor outcomes.
In the early postoperative period, the differential diagnosis of PVT with pulmonary venous occlusion includes primary graft dysfunction (primary graft dysfunction PGD short and longterm outcomes), acute rejection, and infection. The clinical exam findings of right-sided hemiparesis, head CT imaging with left-sided intracerebral hemorrhage, and the CT imaging of the neck with absent left internal carotid artery blood flow make pulmonary venous outflow obstruction the most likely etiology for her hypoxemic respiratory failure.
The clinical presentation is consistent with PGD; however, the postoperative stroke makes pulmonary venous obstruction more likely than PGD (choice A is incorrect).
Infection is also a concern in posttransplantation respiratory failure but again would not be associated with a stroke (choice D is incorrect).
Hyperacute antibody-mediated rejection (AMR) is a form of humoral rejection that occurs in the first 24 h after lung transplantation. Hyperacute AMR occurs in lung transplant recipients who have preformed antihuman leukocyte antigen antibodies, resulting in the production of donor-specific antibodies. The clinical presentation is consistent with hyperacute AMR, but there are no donor-specific antibodies, and the postoperative stroke makes pulmonary venous obstruction more likely than AMR (choice C is incorrect).12345678
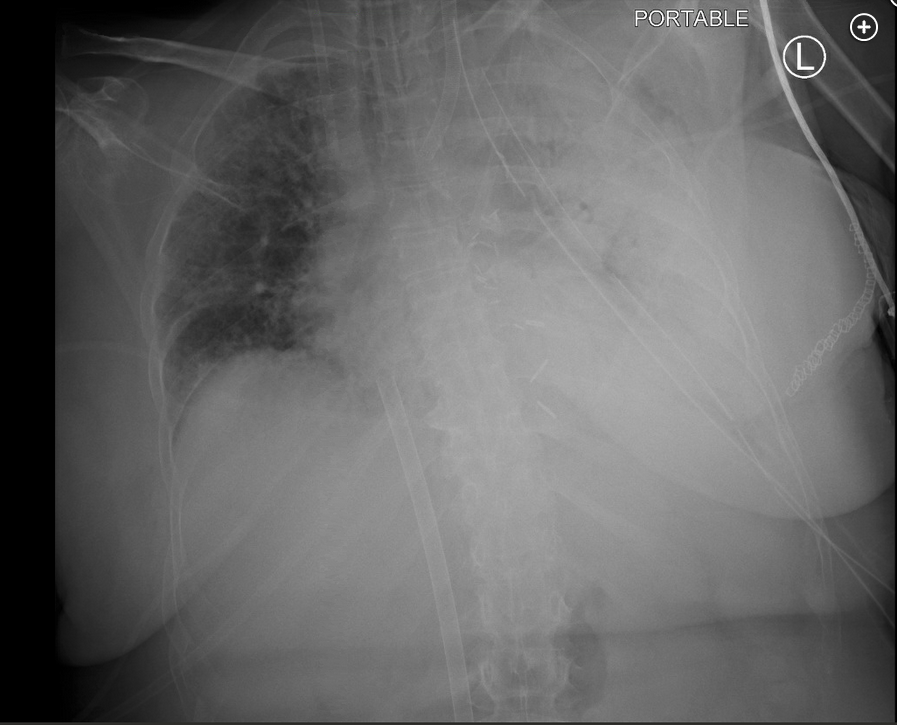
A 50-year-old woman was admitted for left single lung transplant for interstitial lung disease. Her intraoperative course was uncomplicated, with immediate postoperative PaO2 of 306 mm Hg. Upon arrival to the cardiothoracic ICU, she developed acute hypoxemic respiratory failure requiring FiO2 of 1.0, which was associated with new infiltrates in her graft and a PaO2:FiO2 ratio of 89 mm Hg. She was maintained on lung-protective ventilation and placed on venovenous extracorporeal membrane oxygenation (VV-ECMO). No donor-specific antibodies were present. Her oxygenation improved being supported by VV-ECMO, allowing FiO2 to be weaned to 0.40 on the ventilator, but her infiltrates progressed with near-complete opacification of the graft (Figure 1). On postoperative day 1, it was noted that she was no longer spontaneously moving her right upper extremity (RUE) and right lower extremity (RLE). On physical exam, her RUE and RLE did not withdraw from painful stimuli. She underwent emergent head CT scanning. Representative head CT images are shown (Figure 2 and Figure 3).
Which of the following is the most likely etiology for her hypoxemic respiratory failure?
Links to this note
Footnotes
-
Benzimra M, Calligaro GL, Glanville AR. Acute rejection. J Thorac Dis. 2017;9(12):5440-5457. PubMed ↩
-
Denton EJ, Rischin A, McGiffin D, et al. Refractory pulmonary edema caused by late pulmonary vein thrombosis after lung transplantation: a rare adverse event. Ann Thorac Surg. 2016;102(3):e197-e199. PubMed ↩
-
González-Fernández C, González-Castro A, Rodríguez-Borregán JC, et al. Pulmonary venous obstruction after lung transplantation. Diagnostic advantages of transesophageal echocardiography. Clin Transplant. 2009;23(6):975-980. PubMed ↩
-
Schulman LL, Anandarangam T, Leibowitz DW, et al. Four-year prospective study of pulmonary venous thrombosis after lung transplantation. J Am Soc Echocardiogr. 2001;14(8):806-812. PubMed ↩
-
Shah AS, Michler RE, Downey RJ, et al. Management strategies for pulmonary vein thrombosis following single lung transplantation. J Card Surg. 1995;10(2):169-178. PubMed ↩
-
Snell GI, Yusen RD, Weill D, et al. Report of the ISHLT Working Group on Primary Lung Graft Dysfunction, part I: definition and grading-a 2016 consensus group statement of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2017;36(10):1097-1103. PubMed ↩
-
Uhlmann EJ, Dunitz JM, Fiol ME. Pulmonary vein thrombosis after lung transplantation presenting as stroke. J Heart Lung Transplant. 2009;28(2):209-210. PubMed ↩