pulse oximeters inaccuracy in hypoperfusion state and in darker skin tones
- related: ICU intensive care unit
- tags: #literature #icu
The COVID-19 pandemic highlighted the many health equity challenges that persist in modern medicine today, including the performance of common medical monitoring devices. Spurred by initial retrospective reports, carefully controlled prospective data have demonstrated that commercially available pulse oximeters are associated with the greatest risk of occult hypoxemia (defined as an arterial oxygen saturation or SaO2 <88% when oxygen saturation measured by pulse oximetry or SpO2 is >92%) in patients with skin that contains greater degrees of melanin (Fitzpatrick skin type V and VI) in the setting of low-perfusion states.
Pulse oximetry is commonly performed in the ICU as a rapid and noninvasive transcutaneous method to measure blood oxygen saturation. This technique uses a pair of diodes to emit two specific red and near-infrared wavelengths of light that both penetrate tissue well and are absorbed by deoxygenated and oxygenated hemoglobin (660 and 940 nm, respectively). The light that is reflected through the tissue (most commonly, the nail bed of the finger, forehead, nose, or ear lobe owing to capillary density in these locations) is detected by a photodiode, which provides an indirect assessment of the relative amounts of absorbed light at each frequency and is used to calculate the proportion of hemoglobin bound to oxygen. SpO2 detection is based on the fact that arterial blood volume and therefore absorption varies during systole and diastole, while venous blood volume and skin, fat, and bone absorption are nonpulsatile and constant. Pulse oximeters measure the pulsatile blood compartment and calculate an R value, the double-ratio of the pulsatile and nonpulsatile components of red and near-infrared light absorption. A microprocessor uses this ratio, calculated over a series of pulses, to determine SpO2 based on a calibration curve created from healthy volunteers with SpO2 values from 70% to 100% created under controlled conditions.
The FDA requires prescription pulse oximeters to have an accuracy (reported as an accuracy root mean square error) that is within 2% to 3% of arterial blood gas values. This standard means that during device testing, approximately 95% of SpO2 values fall within 4% to 6% of SaO2 measurements. The FDA requires testing cohorts—who are generally healthy individuals—to include a minimum of 2 of 10 subjects or 15% (whichever is larger), and data are collected under ideal conditions.
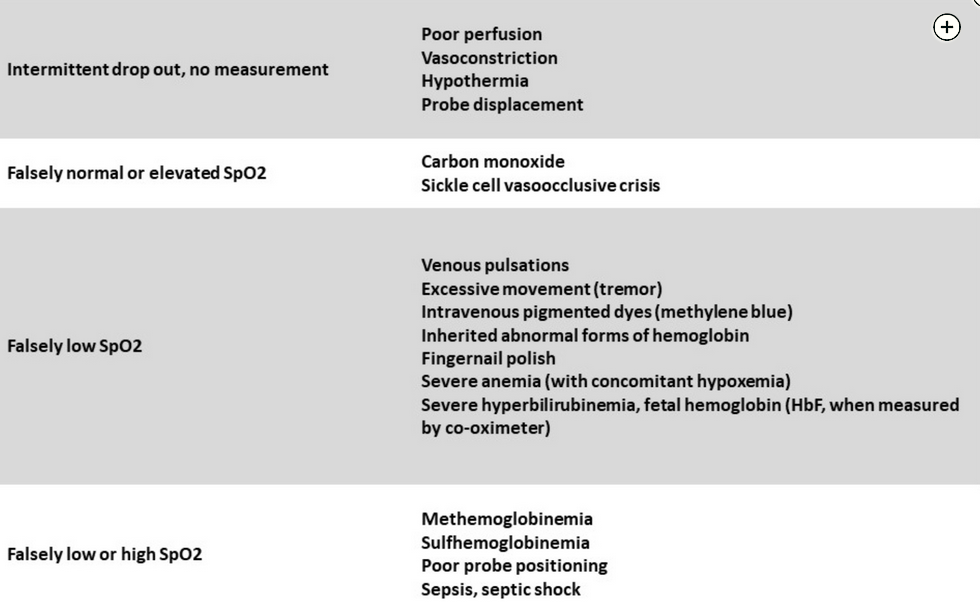
There are many clinical situations in the ICU, however, that introduce SpO2 measurement error (Figure 1) regardless of patient skin pigmentation.
Both retrospective and carefully controlled prospective studies using simultaneous SpO2 and SaO2 sampling have demonstrated both higher and lower SaO2 measurements for a given SpO2 in Black, Asian, and Hispanic populations (greater variance). The risk of occult hypoxemia in these patient populations is greatest in the setting of low-perfusion states. Occult hypoxemia has been associated with delays in treatment in patients with COVID-19 and increased mortality across all racial groups. The FDA issued a safety communication in 2021 that highlighted these concerns, and the lessons learned from its ongoing engagement with key stakeholder groups to develop new standards for pulse oximeter premarketing evaluation may accelerate ongoing efforts to eliminate systemic racism and inequities that unfortunately persist in our health care delivery system.1234567
Links to this note
Footnotes
-
Gottlieb ER, Ziegler J, Morley K, et al. Assessment of racial and ethnic differences in oxygen supplementation among patients in the intensive care unit. JAMA Intern Med. 2022;182(8):849-858. PubMed ↩
-
Henry NR, Hanson AC, Schulte PJ, et al. Disparities in hypoxemia detection by pulse oximetry across self-identified racial groups and associations with clinical outcomes. Crit Care Med. 2022;50(2):204-211. PubMed ↩
-
Seitz KP, Wang L, Casey JD, et al. Pulse oximetry and race in critically ill adults. Crit Care Explor. 2022;4(9):e0758. PubMed ↩
-
Sjoding MW, Dickson RP, Iwashyna TJ, et al. Racial bias in pulse oximetry measurement. N Engl J Med. 2020;383(25):2477-2478. PubMed ↩
-
Valbuena VSM, Merchant RM, Hough CL. Racial and ethnic bias in pulse oximetry and clinical outcomes. JAMA Intern Med. 2022;182(7):699-700. PubMed ↩
-
Wong AI, Charpignon M, Kim H, et al. Analysis of discrepancies between pulse oximetry and arterial oxygen saturation measurements by race and ethnicity and association With organ dysfunction and mortality. JAMA Netw Open. 2021;4(11):e2131674. PubMed ↩