purely ground glass lung nodule
- related: lung mass and cancer
- tags: #literature #pulmonology
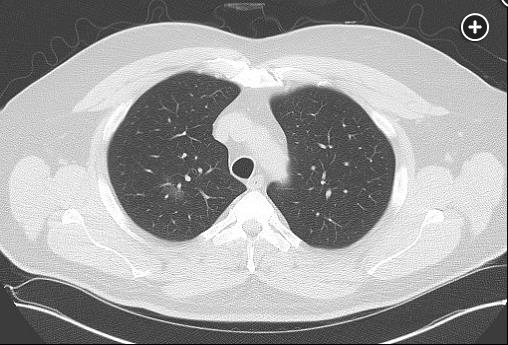
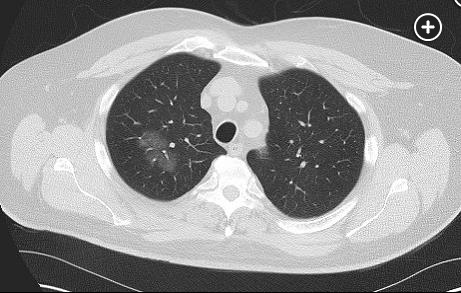
This patient has a very slowly growing pure ground-glass lung nodule. This is most compatible with an adenocarcinoma spectrum lesion, likely adenocarcinoma in situ. As long as the nodule is pure ground glass (ie, it has not developed a solid component), surveillance with chest CT imaging is recommended.
Lung nodules can be divided into solid nodules and subsolid nodules on the basis of their density on chest CT images. Subsolid nodules can be further divided into pure ground-glass and part-solid nodules. Ground glass refers to a nodule density that allows lung architecture to be seen through the nodule. When a subsolid lung nodule is a cancer, it is usually a cancer along the adenocarcinoma spectrum. The density often correlates with disease, where ground-glass density on images represents an adenocarcinoma in situ or minimally invasive adenocarcinoma and a solid part on images represents an invasive adenocarcinoma component. Pure ground-glass nodules smaller than 6 mm in diameter develop into adenocarcinoma less than 1% of the time and, if resected, demonstrate an invasive component less than 5% of the time. An invasive component is found in 70% of those with a solid component greater than 25% of the total nodule size and 45% of those with growth in the solid component. Cancer-specific survival rates of resected ground-glass nodules approaches 100%.
When a subsolid lung nodule is malignant, its behavior is usually more indolent than that of a solid malignant nodule. Growth rates are substantially slower and the spread to regional or distant sites is much less common. When malignant, a solid component develops in a pure ground-glass nodule or grows in a subsolid nodule in the majority of patients within 3 years. The slow growth rate reflects low metabolic activity, which translates into low uptake at fluorodeoxyglucose-PET imaging. The nodule architecture limits the amount of malignant tissue obtained from nonsurgical biopsies, limiting their yield (choice A is incorrect). These features suggest that longer intervals of surveillance can be recommended without detriment to the patient, particularly in patients who are elderly or have significant comorbidities. Videoor robot-assisted thoracoscopic sublobar resection can be considered without biopsy when the nodule evolves in a concerning manner at imaging.
Current guidelines outline a patient-centered approach to the management of subsolid lung nodules, with flexibility to individualize care. Guidelines suggest a pure ground-glass nodule smaller than 6 mm in diameter does not require additional testing or monitoring. A ground-glass nodule 6 mm or larger can be followed up with a chest CT scan in 6 to 12 months and then every 2 years for 5 years if it remains stable. Part-solid nodules should be managed based on the size of the solid component. Surveillance with a chest CT scan should occur in 6 months if the solid component is smaller than 6 mm and in 3 months if the solid component is 6 to 8 mm, and management should follow solid nodule guidelines when the solid component is larger than 8 mm. The development or growth of a solid component of the nodule is a concerning finding that should lead to more frequent surveillance imaging, nonsurgical biopsy, or surgical resection based on the size of the solid component of the nodule. Growth of the ground-glass component alone does not suggest a malignancy is becoming invasive and thus does not require more aggressive management (choice C is incorrect).1