reexpansion pulmonary edema happens more in chronic effusion and can be bilateral
- related: pleural effusion
- tags: #literature #pulmonology
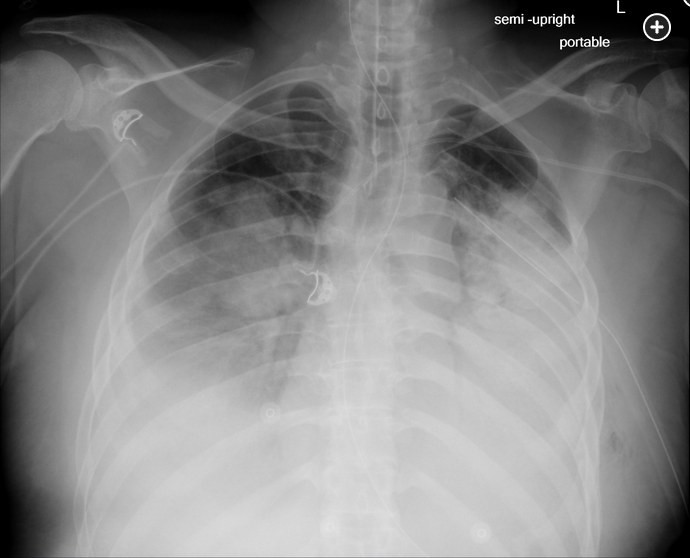
The 2-month history of this patient’s lung collapse places him at increased risk for reexpansion pulmonary edema. In patients with chronic collapse of a lobe or whole lung, rapid reexpansion can abruptly increase pulmonary blood flow, leading to stress capillary failure on the affected side. This endothelial injury leads to the recruitment and activation of inflammatory cells and the release proinflammatory cytokines that can increase the permeability in both the affected lung and in the contralateral lung.123
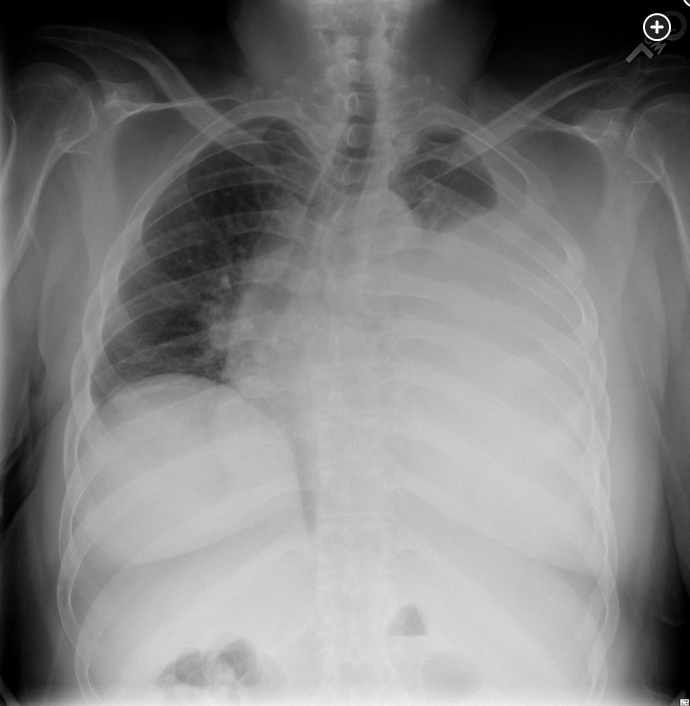
A 44-year-old man was kicked in the chest during an altercation 2 months ago and has had persistent left anterolateral chest wall pain and shortness of breath. He has had no fever or chills. His presenting chest radiograph today is shown (Figure 1). Following tube thoracostomy, 2 L of bloody pleural fluid are removed, and a second chest radiograph is obtained (Figure 2). The hematocrit of the pleural fluid is 10%, while the peripheral blood hematocrit is 43%. The pleural fluid has a pH of 7.15, WBC count of 7,200/μL (7.20 × 109/L), and lactate dehydrogenase of 1,533 U/L (25.60 µkat/L). Gram stain shows no organisms. Over the next 4 h, his shortness of breath worsens. His SpO2 is now 70% on 50% oxygen via face mask. Following emergent intubation, a repeat chest radiograph is obtained (Figure 3). The most likely explanation for this patient’s clinical deterioration is which of the following?
Links to this note
Footnotes
-
Kim JJ, Kim YH, Choi SY, et al. Contralateral reexpansion pulmonary edema with ipsilateral collapsed lung after pleural effusion drainage: a case report. J Cardiothorac Surg. 2015;10:68. PubMed ↩
-
Walter JM, Matthay MA, Gillespie CT, et al. Acute hypoxemic respiratory failure after large-volume thoracentesis. Mechanisms of pleural fluid formation and reexpansion pulmonary edema. Ann Am Thorac Soc. 2016;13(3):438-443. PubMed ↩