REM sleep and pulmonary disorders
- related: Sleep and Sleep Disordered Breathing
- tags: #literature #pulmonology
In adults, approximately 20% to 25% of total sleep time is spent in REM sleep. REM sleep is more prevalent during the second half of the sleep period and is characterized by intermittent rapid eye movements, low or no muscle tone (ie, atonia), and the propensity to dream vividly. The atonia characterizing REM sleep also involves intercostal and accessory muscles of respiration. Moreover, REM sleep is also characterized by a significant decrease in hypoxic and hypercapnic ventilatory drive compared with non-REM sleep and wakefulness. Accordingly, patients with COPD may experience hypoventilation and hypoxemia only during REM sleep (choice A is correct). In patients with severe hypercapnic COPD, hypoventilation can worsen during sleep, particularly during REM sleep. In patients with nonhypercapnic COPD, however, hypoventilation and hypoxemia may be present only during REM sleep.
Distinguishing between wakefulness, non-REM sleep (stages 1, 2, and 3), and REM sleep requires EEG, electro-oculography (EOG), and electromyography (EMG), which are available in polysomnography laboratories. Home sleep apnea testing devices lack EEG, EOG, and EMG and thus cannot provide sufficient data for accurate staging of sleep. Various technologies and proprietary algorithms have been used by commercially available consumer wearable devices to measure sleep, including sleep stages. Ultimately, however, accurate staging of sleep requires EEG, EOG, and EMG.
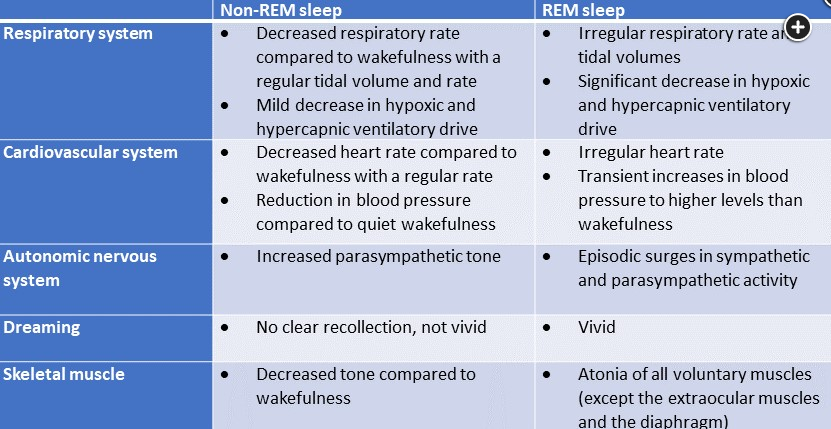
Figure 1 compares important physiologic differences between REM and non-REM sleep. REM sleep physiology is relevant to several disorders:
- Pulmonary disease: REM-related atonia also includes intercostal and accessory muscles of respiration. Patients with abnormal respiratory mechanics (eg, in COPD, kyphoscoliosis, neuromuscular disease) rely on these accessory muscles of respiration during sleep to maintain an adequate level of ventilation. During REM sleep, these patients may develop significant hypoventilation and hypoxemia.
- OSA: Because of loss of muscle tone, upper airway patency becomes more compromised during REM sleep, which can significantly worsen the frequency and duration of obstructive apneas and hypopneas compared with non-REM sleep. Moreover, given the significantly reduced hypoxic and hypercapnic ventilatory drive, hypoxemia and hypercapnia can be more profound during REM sleep in patients with OSA. In some patients, OSA can occur exclusively in or become significantly more severe during REM sleep.
- Narcolepsy: Patients with narcolepsy can have very-early-onset REM sleep during their sleep period (a latency of less than 15 min after sleep onset as opposed to a normal REM sleep latency of 90-120 min). In patients with narcolepsy, REM sleep can also occur during brief daytime naps. Short sleep latency during the patient’s typical sleep period or intrusion of REM sleep during short naps are features of the disease used to make the diagnosis by polysomnography and multiple sleep latency test. Cataplexy is present in narcolepsy type 1; this condition consists of intrusion of REM sleep during wakefulness with skeletal muscle hypotonia or atonia as a characteristic feature.
- REM sleep behavior disorder (RBD): In RBD, the normal muscle atonia that is characteristic of REM sleep is incomplete or absent. Since REM sleep is also characterized by vivid dreaming, patients may have dream enactment that leads to self-injury or may injure their bed partner. In the elderly, RBD can be a prodromal syndrome of alpha-synuclein neurodegeneration such as Parkinson disease, multiple system atrophy, or dementia with Lewy bodies. In younger individuals, other etiologies of RBD should be considered, such as narcolepsy or a side effect of antidepressants that are selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors.
During non-REM sleep, breathing is more stable, and there is minimal impact on hypoxic and hypercapnic ventilatory drive as compared with wakefulness, which is why the risk of hypoventilation and hypoxemia during non-REM sleep is lower than during REM sleep (choices B, C, and D are incorrect).1