reperfusion pulmonary edema following thromboendarterectomy
- related: Pulmonary Diseases
- tags: #literature #pulmonology
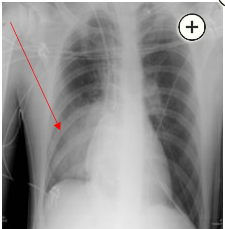
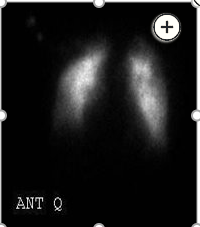
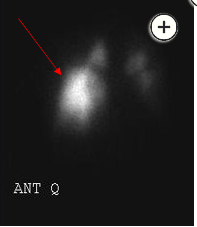
Reperfusion pulmonary edema is a complication of pulmonary thromboendarterectomy that occurs in approximately 30% of patients, typically in regions where proximal chronic thromboemboli have been resected (choice D is correct). The diagnosis is suggested by the chest radiograph showing airspace disease in the right lower lobe, where the patient’s most significant lesions were removed (Figure 4). Although not generally ordered in the acute setting, a repeat radionuclide perfusion scan was obtained in this patient and showed increased blood flow and exudation of the tracer into alveolar spaces of the right lower lobe, further confirming the diagnosis (Figure 5).
Reperfusion pulmonary edema typically develops within the first 72 h after pulmonary thromboendarterectomy or balloon pulmonary angioplasty and can range in severity from mild to life-threatening. Treatment is largely supportive, with supplemental oxygen; mechanical ventilation; and, in severe cases, extracorporeal membrane oxygenation. Some data suggest that inhaled vasodilators may be beneficial, presumably by dilating vasculature in better ventilated portions of the lung to improve ventilation-perfusion matching and by shunting blood flow away from injured areas of the lung, thus decreasing pulmonary edema formation due to reperfusion in those areas. Unfortunately, there is no mechanism to identify preoperatively the precise risk of reperfusion pulmonary edema in a specific patient, and the complication is not reduced by prophylactic low tidal volume ventilation vs higher tidal volumes.
While acute mitral regurgitation can cause localized pulmonary edema due to the regurgitant jet interfering with pulmonary venous inflow to the left atrium, this typically occurs in the right upper lobe, which is not the case in this patient (choice A is incorrect). Allergic reactions to anesthetics may produce bronchospasm or pulmonary edema but should not produce sequelae that are limited to a single lobe (choice B is incorrect.) Pulmonary thromboembolism should produce no change or produce areas of relative lucency on the chest radiograph rather than the localized area of higher attenuation in the right lower lobe that was seen in this patient (choice C is incorrect.)