rheumatoid arthritis RA CT image findings
- related: rheumatoid arthritis
- tags: #literature
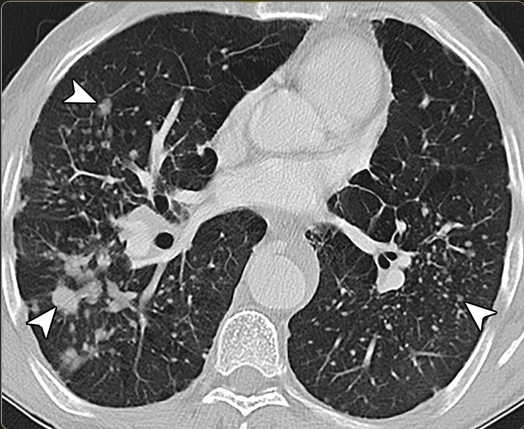
Usual interstitial pneumonia and nonspecifici interstitial pneumonia
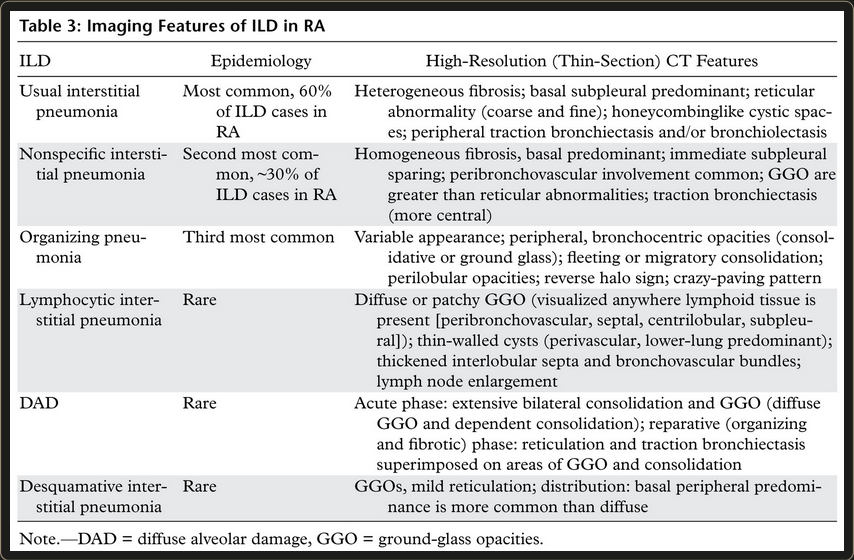
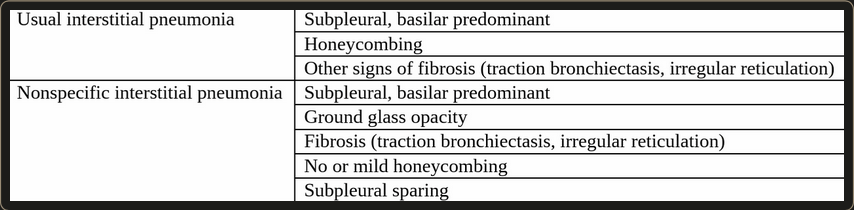
“Although often having different appearances, in some patients, UIP and NSIP may be difficult to differentiate using HRCT. In particular, the fibrotic subtype of NSIP can closely resemble UIP… In UIP, honeycombing is a significant finding, whereas in NSIP, it is either absent or minimal in extent. The greater the severity of fibrosis in the absence of honeycombing, the more likely NSIP becomes. Subpleural sparing strongly suggests NSIP over UIP. While the presence of GGO is more common with NSIP, it is not specific in distinguishing NSIP from UIP. Keep in mind that in patients with CTD, findings typical of both NSIP and UIP may coexist.”1
Organizing pneumonia
LIP
- Diffuse lymphocytic infiltrate
- Lower lobe predominant thin-walled cysts adjacent to vessels (perivascular distribution)
- More common in RA with secondary Sjögren syndrome2
Drug induced lung disease
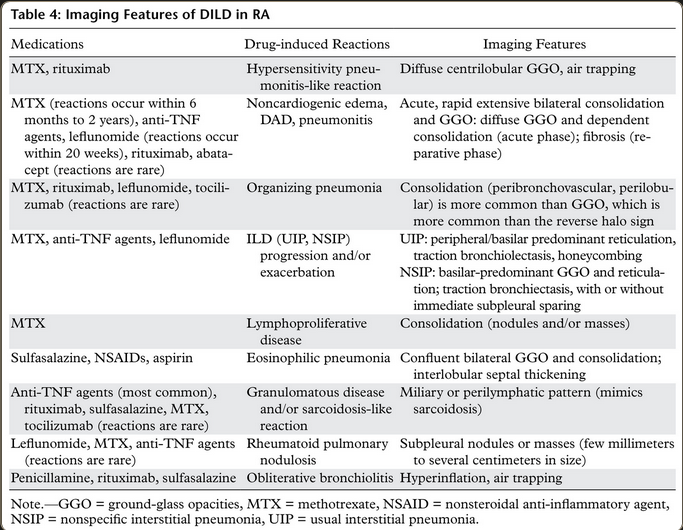
- Most common with methotrexate due to widespread use
- 3-18% of RA patients treated with methotrexate
- Methotrexate pneumonitis can be life-threatening
- Cough, dyspnea, fever, widespread crackles, and pulmonary opacities
- Acute to subacute up to 2 months
- 50% within 4 months of methotrexate initiation
- Nonspecific image and histologic findings2
- Immediate withdrawal of methotrexate and the early steroid3
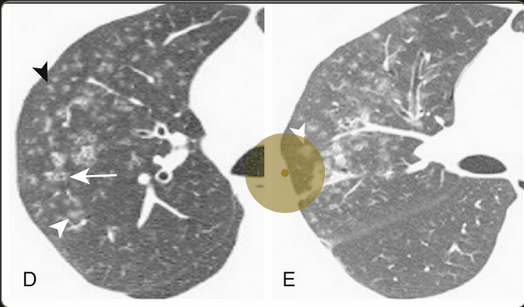
Bronchiolitis obliterans and Follicular bronchiolitis
- Destruction of the bronchiolar wall
- Formation of granulation tissue
- Eventual replacement of the bronchiole by fibrous tissue
- Airflow obstruction, especially nonsmokers
- Follicular bronchiolitis: localized lymphoid infiltration of bronchioles.
- Centrilobular nodules of GGO. Air trapping and mosaic perfusion may also be present.3
- constrictive bronchiolitis is small airway disease
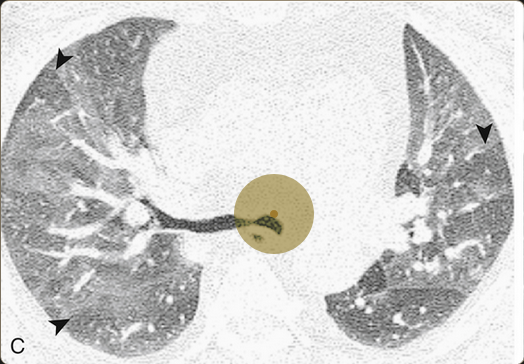
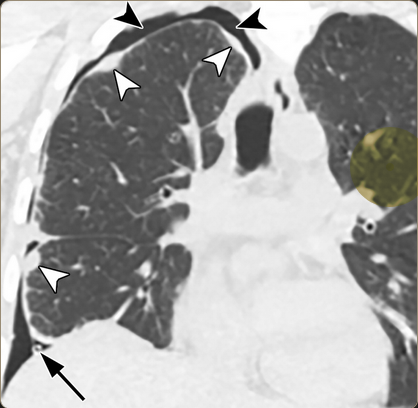
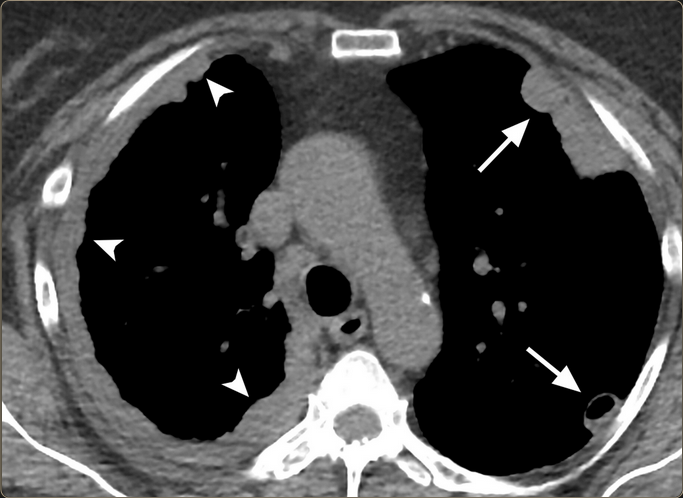
Pulmonary rheumatoid nodules
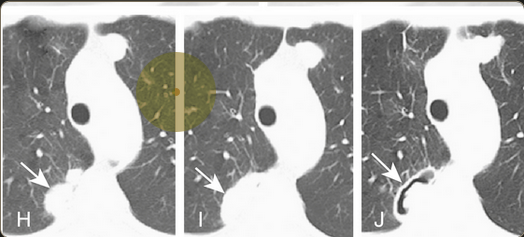
- Single or multiple
- Found on CXR in less than 1% of RA patients
- Often precede the development of systemic disease
- Well circumscribed, varying in size
- Central necrosis surrounded by fibrosis and lymphocytic infiltration
- Cavitation and rupture can lead to hemoptysis, pneumothorax3
Caplan syndrome

- Also known as rheumatoid pneumoconiosis
- Pulmonary nodules in patients with RA with a history of work inhalation exposure
- Coal, silica, rarely asbestos
- Similar to rheumatoid nodules but also contain rings of dust particles and a zone of active inflammation
- May join into larger nodules, with progressive fibrosis
- Cavitation and calcification are common 2
Pulmonary arterial hypertension and vasculitis
- relatively rare
Pleural diseases
- Rheumatoid pleuritis: pleuritic chest pain
- Pleural effusion
- Trapped lung and entrapped lung: dyspnea, fever out of proportion to effusion
- Empyema: especially if on chronic immunosuppression
- Bronchopleural fistula with pneumothorax or hemopneumothorax
Links to this note
-
pulmonary nodule differential diagnosis
- Autoimmune have multiple causes include rheumatoid arthritis (rheumatoid arthritis RA CT image findings), vasculitis, sarcoid, amyloidosis.