risk of lung resection
- related: lung mass and cancer
- tags: #literature #pulmonology
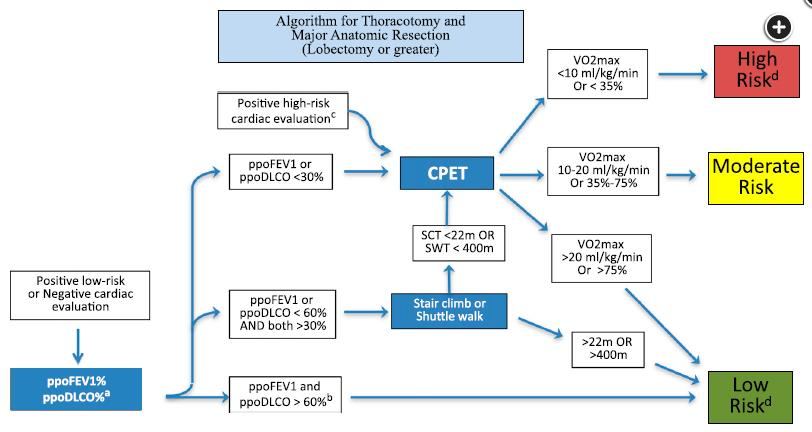
- Figure courtesy of CHEST guideline preoperative risk assessment algorithm. Brunelli A, Kim AW, Berger KI, Addrizzo-Harris DJ. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: Diagnosis and management of lung cancer. 3rd ed. American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(suppl 5):e166S-190S.
- ppo predicted post operative
The risk of pulmonary complications from lung resection correlates with the proportion of functional lung that is resected. In this patient with severe, upper zone predominant emphysema, resection of healthier lung tissue in the lower lobes will lead to a greater reduction in her lung function than if the upper lobes required resection. This translates into a higher risk of nearand long-term pulmonary complications (choice D is correct). If the lung cancer is in the upper lobes in a patient with severe heterogeneous emphysema, it is possible that resection could lead to a lung volume reduction effect.
With this balance of relative benefit and harm in mind, the risk of complications from resection are typically categorized as low, moderate, and high, rather than being considered an absolute indication or contraindication for resection. Pulmonary function and cardiopulmonary fitness testing results have correlated with the risk of complications. Algorithms, such as in the CHEST guidelines (Figure 3), use percent predicted FEV1 and Dlco, predicted postoperative FEV1 and Dlco (by segment methods = preoperative value x [total segments - segments to be resected]/total segments; or quantitative perfusion imaging), low-tech exercise testing (eg, shuttle walk, stair climb, 6-min walk), and cardiopulmonary exercise testing, to assist with the evaluation of risk. Using this algorithm a peak VO2 of 17 mL/kg/min (80% predicted for the patient in this question) would place the patient at low to moderate risk for complications (choice A is incorrect). The FEV1 of 45% predicted would equate to a predicted post operative (ppo) FEV1 of 33% to 36%, and the Dlco of 42% predicted a ppoDlco of 31% to 33%, depending on whether a lobectomy or composite basilar segmentectomy was required. These values alone are not adequate to assign a level of risk, requiring at least a low technology exercise test be performed, though they suggest that the risk is not low (choices B and C are incorrect).
For the patient in this question, the testing performed suggests a low to moderate risk of resection. A more nuanced evaluation might lead to increased concern. In addition to resecting the healthier portion of her lung, the cardiopulmonary exercise test suggested ventilatory limitation at peak exercise. The lack of breathing reserve is concerning for complications from lung resection. She also has a history of requiring oxygen after a respiratory illness, and she desaturated during her exercise test. The location and size of her cancer suggest stereotactic body radiotherapy (SBRT) would be a reasonable alternative to surgery. The risks and benefits of surgery and SBRT were discussed with her. Her value set favored minimizing the risk of her treatment, so SBRT was offered.1