SEEK CPET examples
- related: cardiopulmonary exercise test CPET
- tags: #literature #pulmonology
Case 1
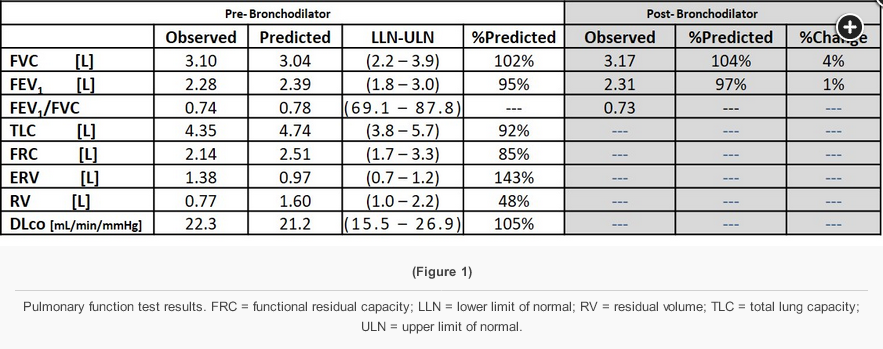
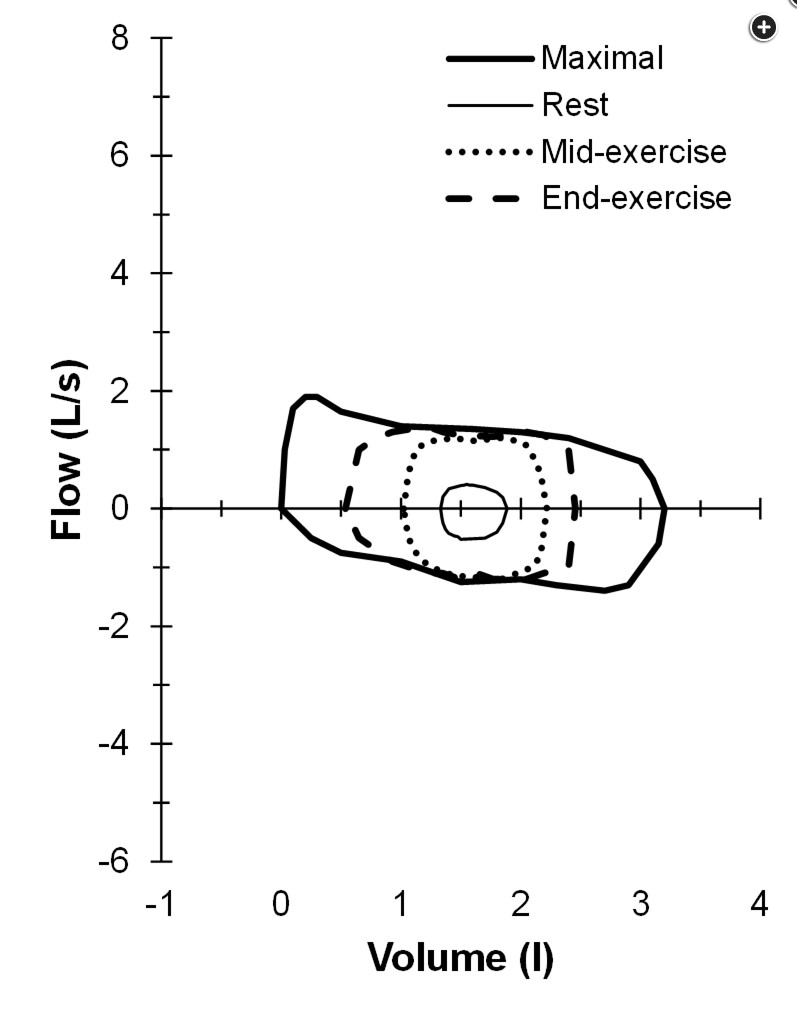
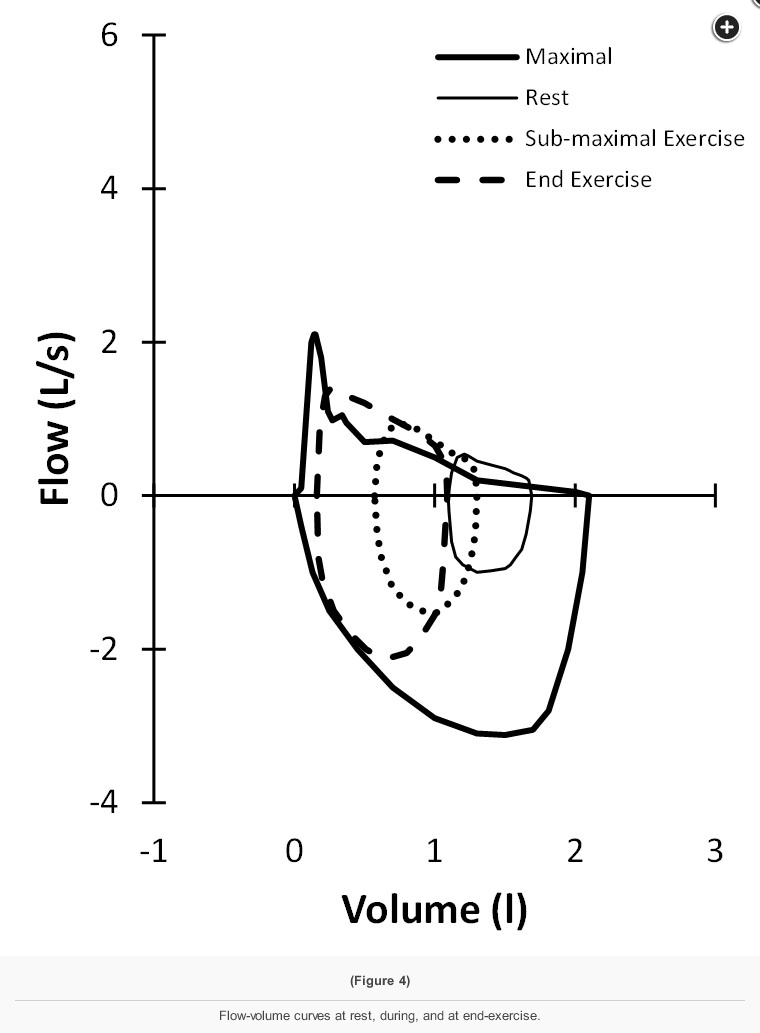
A 54-year-old woman is referred for cardiopulmonary exercise testing (CPET) related to investigation of exertional shortness of breath and activity limitation. Her symptoms began 3 years prior when she noticed difficulty participating in adult recreational soccer, and she now finds herself short of breath after climbing two or three flights of stairs. She also notes cough for the past 5 years and occasional wheezing with vigorous exertion. She tried albuterol for her symptoms but did not notice any improvement. She reports no hemoptysis, sputum production, chest pain, orthopnea, or palpitations. The remainder of the clinical history is negative except for periodic heartburn that responds to antacids and diet modification. She is currently on no medications and is a lifelong nonsmoker. Her BMI is 24.7 kg/m2, her vital signs are normal, and there are no significant murmurs or wheezes on physical examination. An ECG and chest radiograph are normal. Pulmonary function test results are shown (Figure 1).
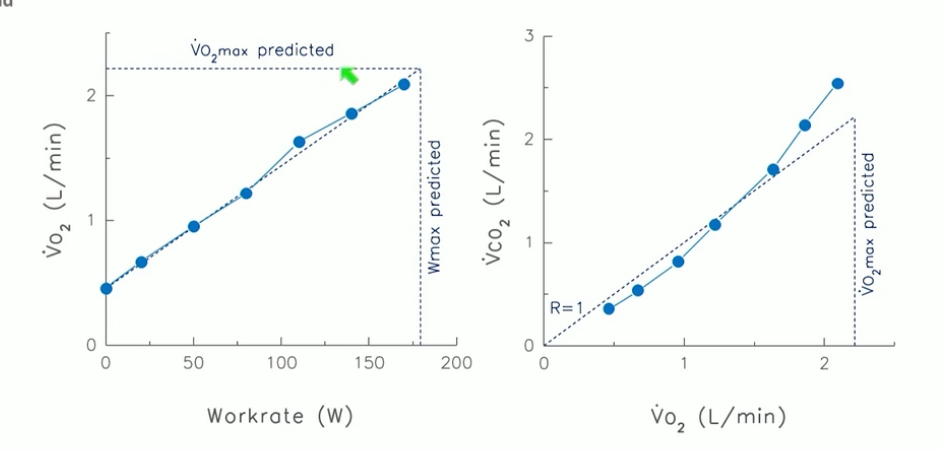
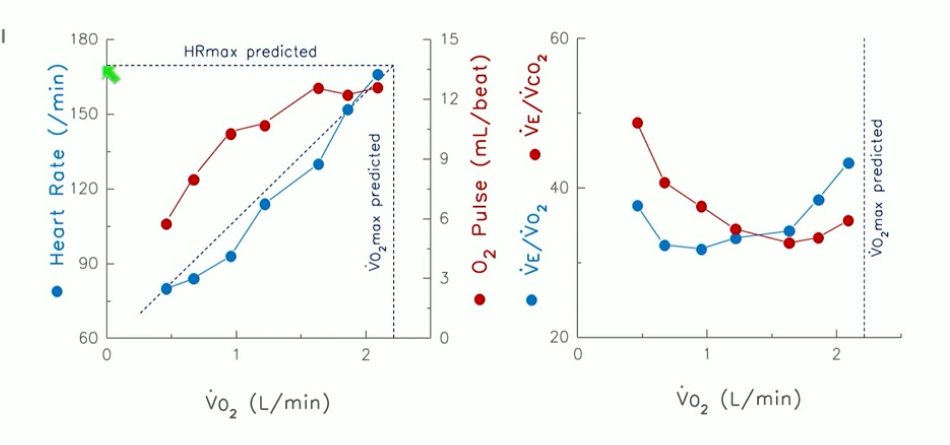
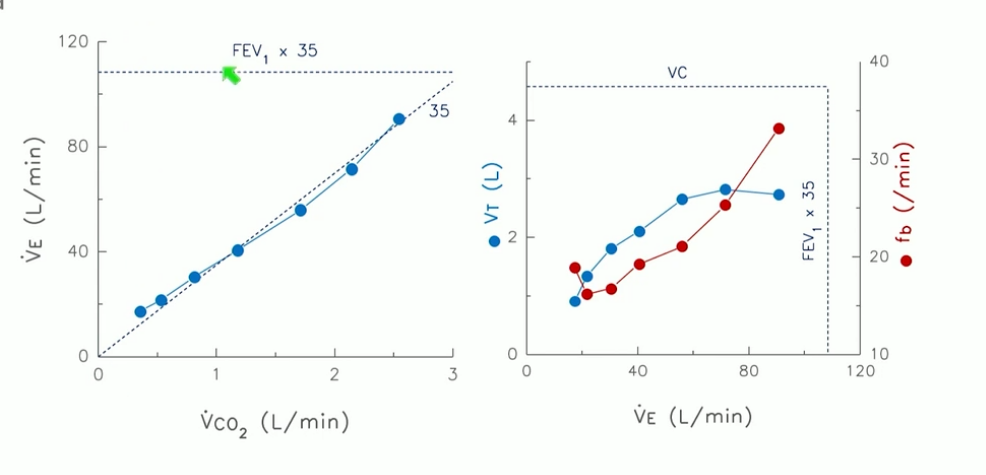
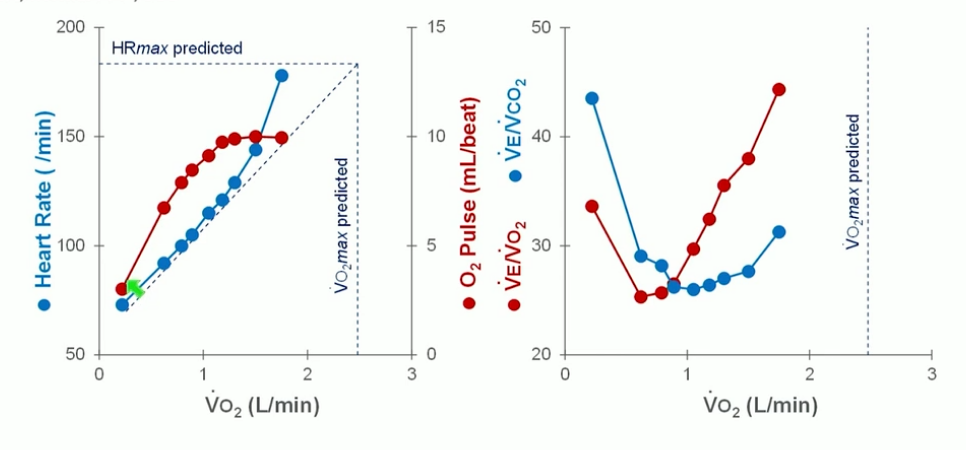
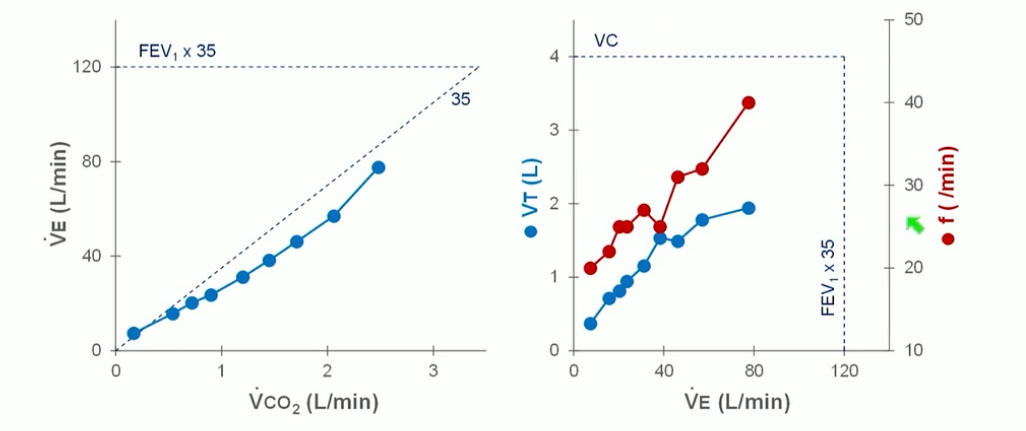
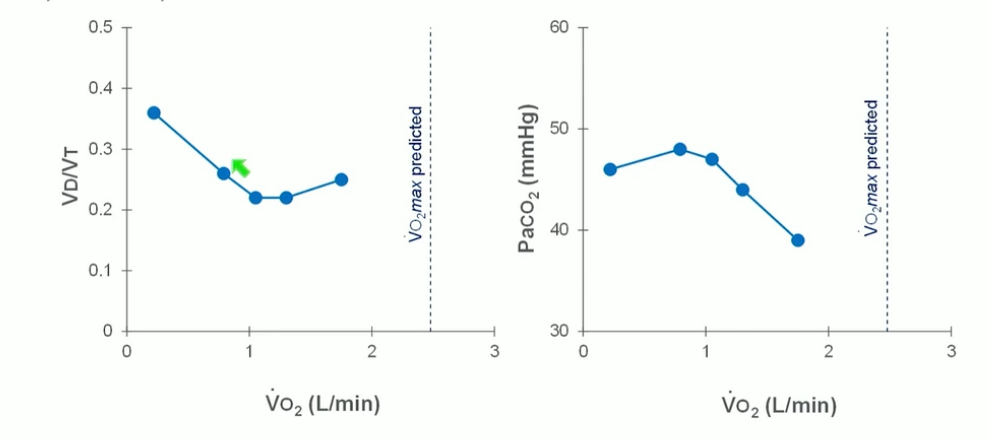
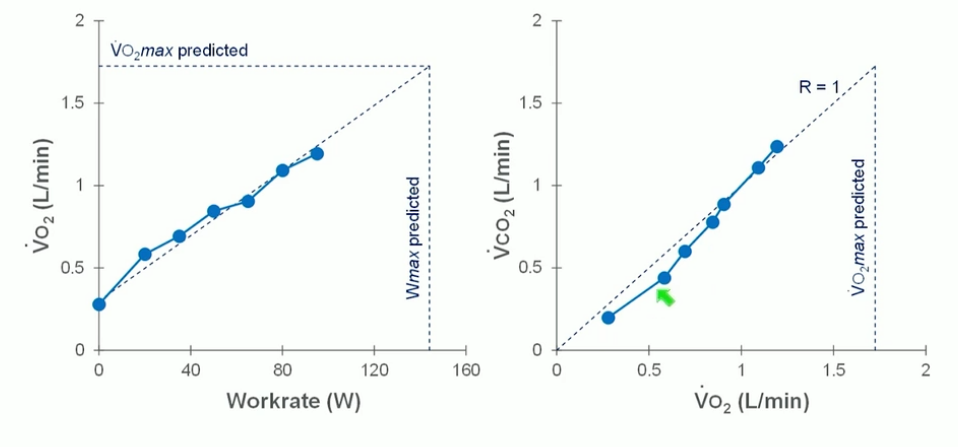
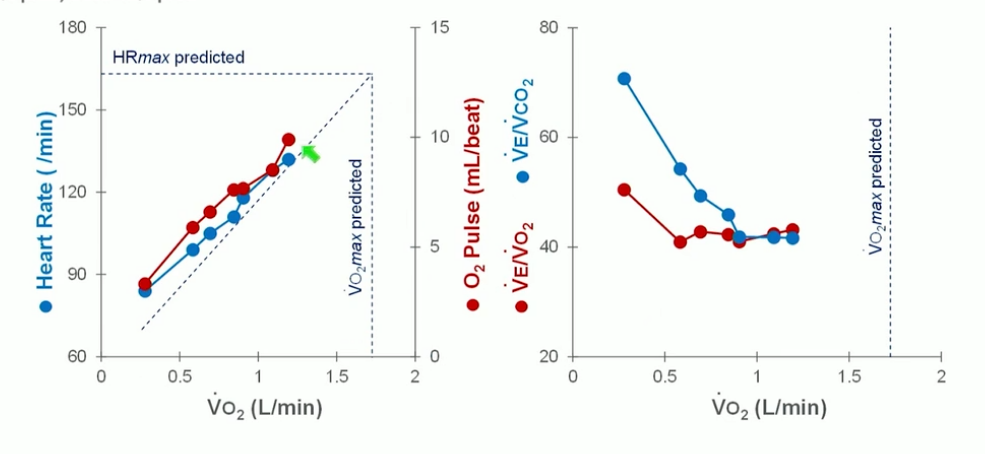
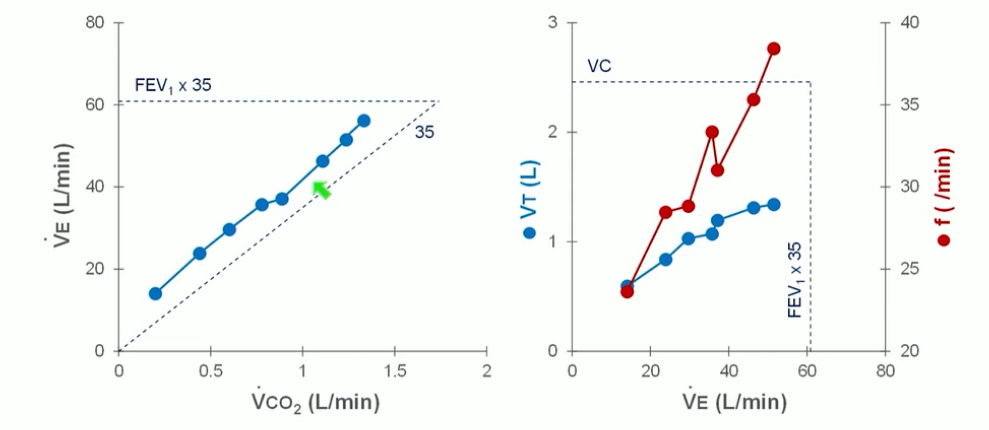
The patient undergoes CPET on an upright bicycle ergometer while breathing room air using an incremental ramp protocol of 15 W/min. CPET results are shown (Figure 2, Figure 3, and Figure 4).
Monitoring with 12-lead continuous ECG revealed no arrhythmias, significant ST segment, or T-wave changes. The patient reported discontinuing exercise because of shortness of breath, and she had no complaints of chest pain, palpitations, or presyncope. Spirometry performed following exercise was unchanged from pre-exercise values.
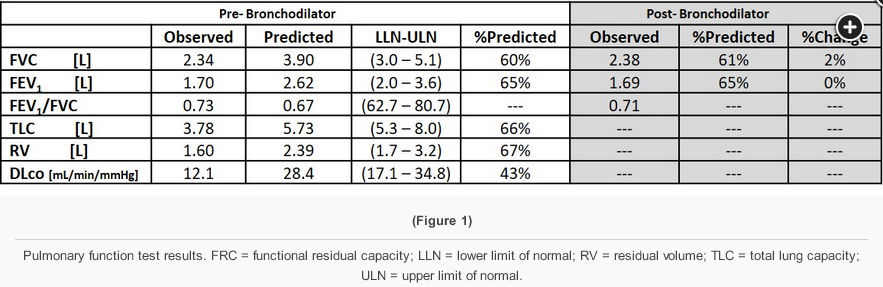
The results from these investigations are most consistent with the patient discontinuing exercise from which of the following?
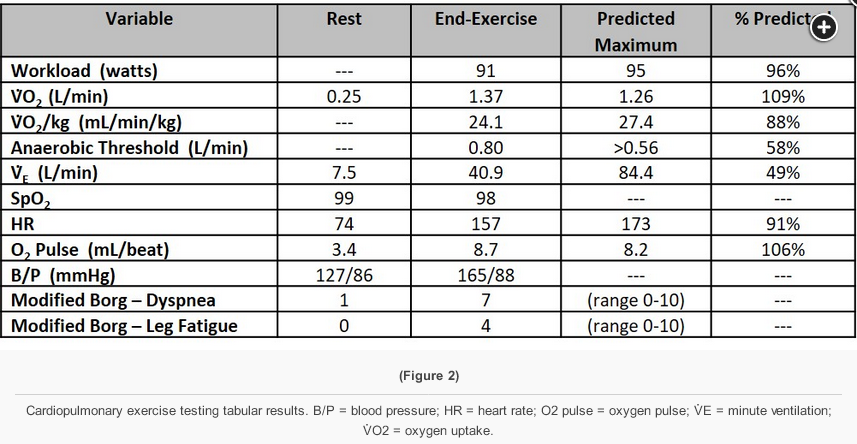
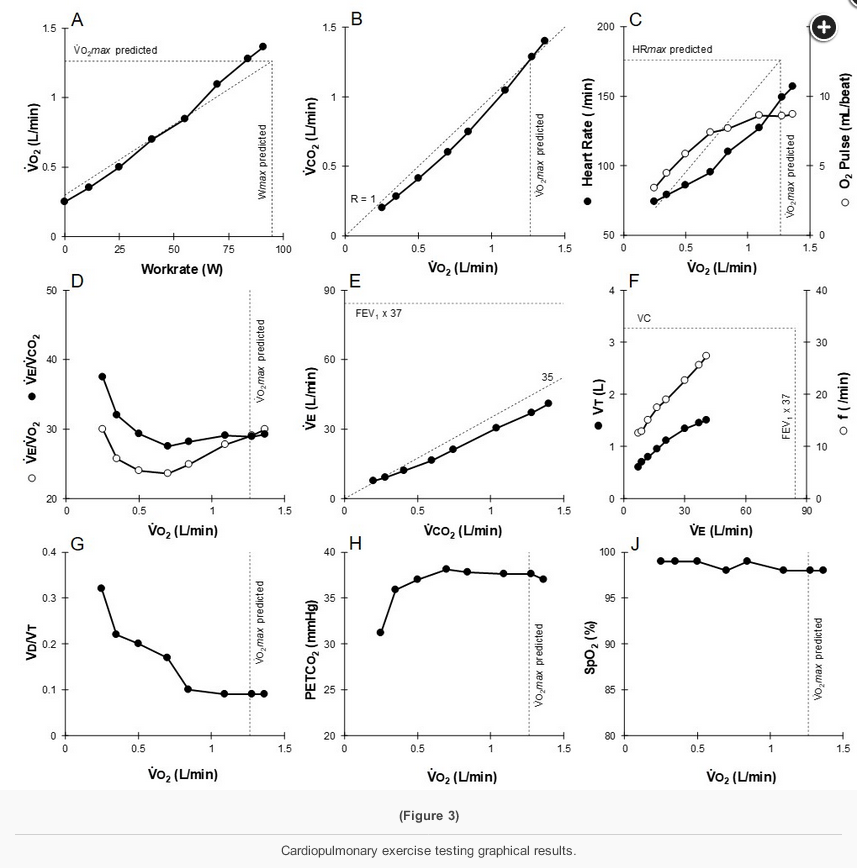
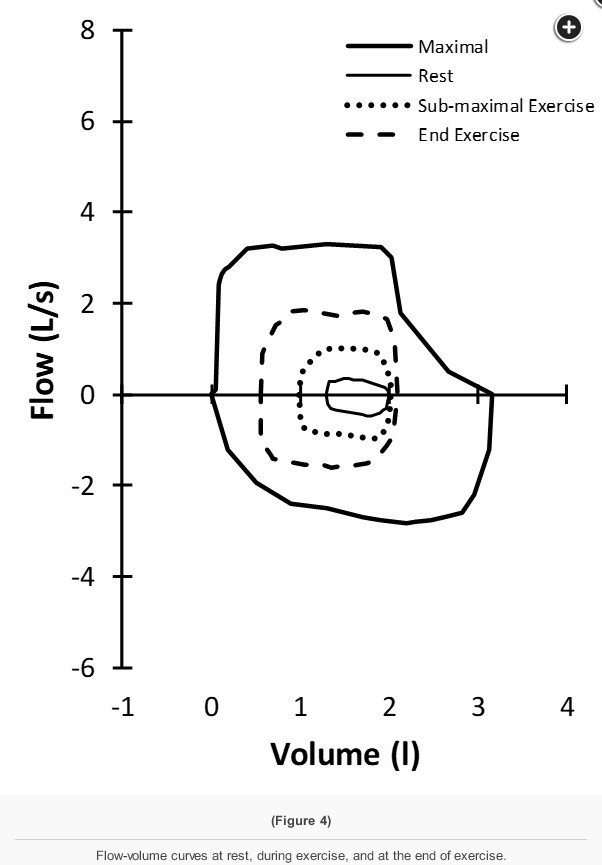
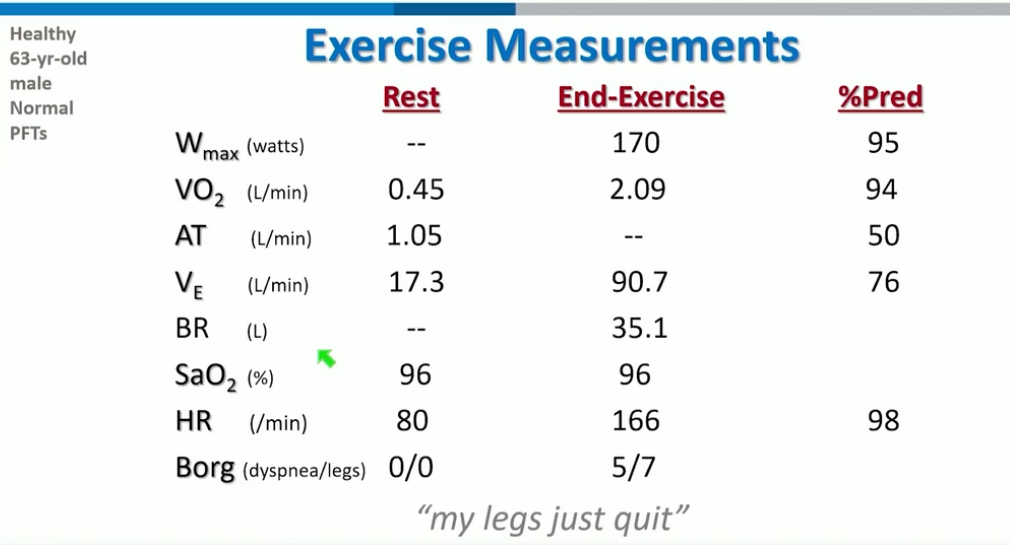
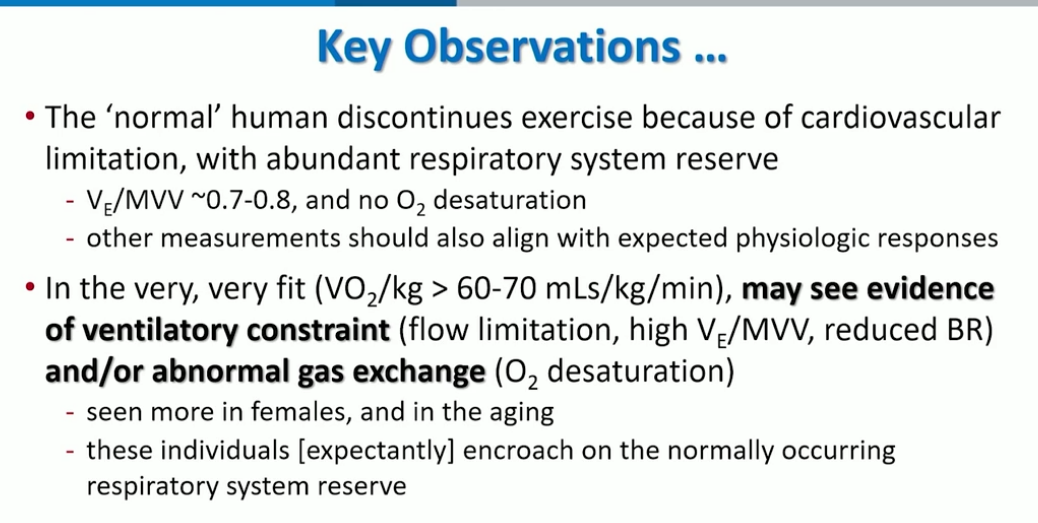
This patient demonstrates normal work (end-exercise workload >90% predicted) and aerobic capacity (peak V̇O2 >90% predicted), a normal anaerobic threshold (>40% predicted maximal peak V̇O2), near maximal heart rate (>90% predicted maximal heart rate), and an appropriate increase in BP during exercise with a normal O2 pulse. In addition, there is significant ventilatory reserve at the end of exercise (V̇E /MVV 49% predicted) (Figure 2 and Figure 3, panel E), normal gas exchange with no oxygen desaturation, and no evidence of significant expiratory or inspiratory flow limitation on tidal flow-volume (f-v) curves during exercise (Figure 4). The breathing pattern during exercise is normal (Figure 3, panel F), the ventilatory equivalents for both O2 and CO2 are normal (Figure 3, panel D), and estimated dead space ventilation falls appropriately during exercise (Figure 3, panel G). This constellation of findings, with the absence of other significant abnormalities, is most consistent with normal exercise physiology and performance (choice C is correct). Even though work and aerobic capacity are normal, it is possible this patient could have exercised more as heart rate reserve was still present at the end of exercise (Figure 2).
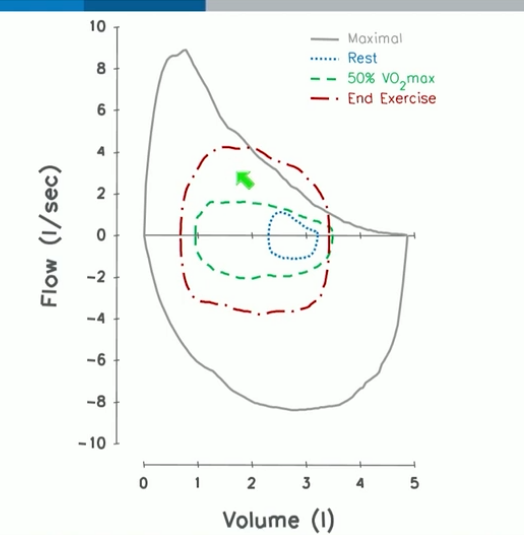
The resting f-v curve is abnormal (Figure 4), with flattening of the expiratory curve at a flow of approximately 3.5 L/min. The maximal inspiratory curve does not demonstrate such flattening, so this is suggestive of variable intrathoracic central airway obstruction. But, importantly, in this patient, the maximal tidal f-v curve (Figure 4, dashed line) does not encroach on the maximal curve (Figure 4, solid thick line) during exercise—that is, there is expiratory flow reserve at the end of exercise (choice A is incorrect). It is possible the complex sensation of dyspnea experienced by this patient may be heightened because of the impaired maximal expiratory flow, but this finding is not physiologically limiting the patient’s exercise performance.
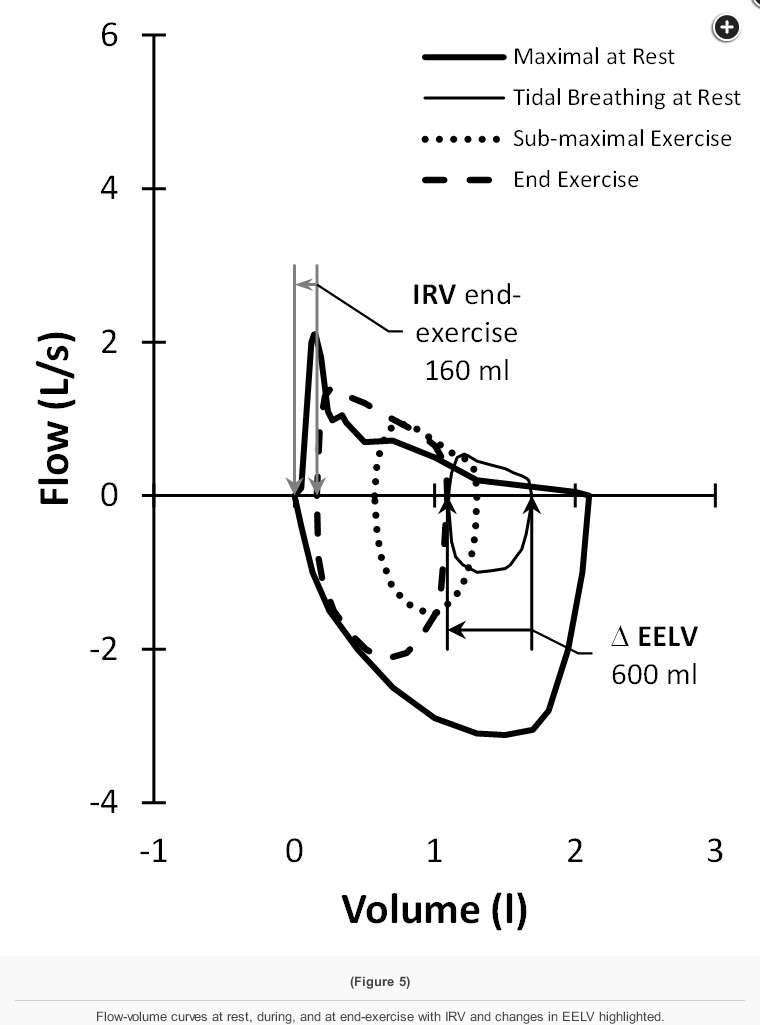
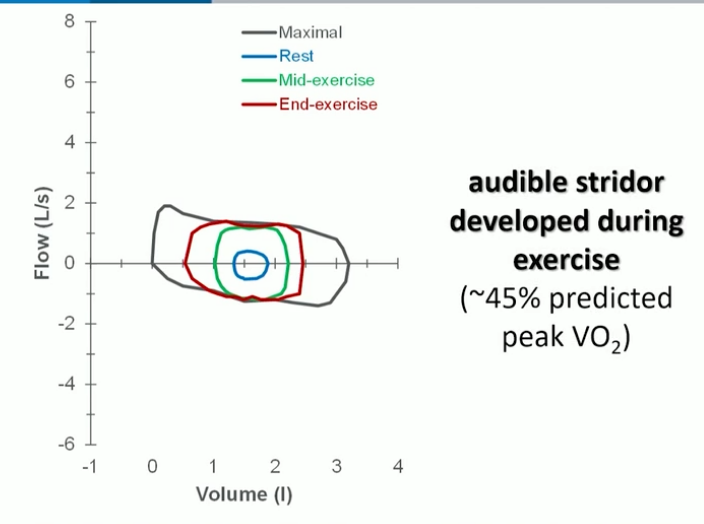
Figure 5 demonstrates findings on exercise tidal f-v curves characteristic of significant central airway obstruction. There is expiratory and inspiratory flow limitation at mid-exercise (dotted line) such that further increases in ventilation at the end of exercise (dashed line) are achieved only by a horizontal decrease in end-expiratory lung volume and an increase in end-inspiratory lung volume—that is, maximal expiratory and inspiratory flows do not change after mid-exercise.
- Figure 5
Although deconditioning is a common finding in patients with unexplained exertional dyspnea, this patient exhibited normal work and aerobic capacity (choice B is incorrect). Patients with deconditioning also more characteristically demonstrate an exaggerated heart rate during exercise unless impaired exercise performance is associated with a physiologically submaximal effort. There is no history of cardiac disease, cardiac examination is normal, and the resting ECG is normal. The lack of a tachycardic heart rate response, the normal oxygen pulse during exercise, and the lack of other abnormalities consistent with impaired cardiac function exclude inotropic cardiac dysfunction as the etiology most responsible for exercise limitation in this patient (choice D is incorrect).
This patient underwent additional investigations that led to a diagnosis of subglottic stenosis of unknown etiology, although significant gastroesophageal reflux was documented. Treatment of the gastroesophageal reflux did lead to near-complete resolution of her cough. She was been followed up for 1 year after these investigations, and her clinical status remains stable.
Case 2
A 72-year-old woman is referred for cardiopulmonary exercise testing (CPET) in the setting of severe COPD and marked activity limitation. The referring physician believes her management is optimized and is questioning whether there are other potential factors contributing to her impaired exercise. She stops walking after one block because of shortness of breath. She has a 50 pack-year smoking history but quit smoking 7 years ago when she was diagnosed. Her vaccinations are up to date, and she has no other known medical conditions except for osteoarthritis affecting her hips and knees. Her inhaled therapy is a once-a-day long-acting muscarinic antagonist/long-acting beta agonist (LAMA/LABA) combination and as-needed salbutamol, which she uses 3-4x/day. Her inhaler technique is excellent.
On physical examination, BMI is 24.5, Spo2 breathing room air is 96%, and vital signs are normal. Breath sounds are reduced to both lung fields, but there are no crackles or focal signs of consolidation. She has no significant murmurs or extra heart sounds, and there is no peripheral edema. A chest radiograph reveals hyperinflation and reduced vascular markings but no other abnormalities. An electrocardiogram is normal. Pulmonary function test results are as follows (Figure 1):
The patient undergoes cardiopulmonary exercise testing on an upright bicycle ergometer while breathing room air utilizing an incremental ramp protocol of 5 watts/min. CPET results are shown (Figure 2, Figure 3, and Figure 4):
Twelve-lead continuous ECG monitoring revealed no arrhythmias, significant ST segment, or T wave changes. The patient reported discontinuing exercise because of shortness of breath, with no chest pain, palpitations, or presyncope.
The results from these investigations are most consistent with this patient’s discontinuation of exercise from which of the following?
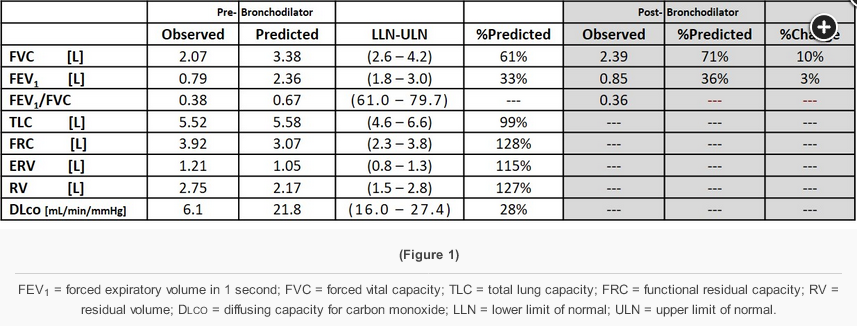
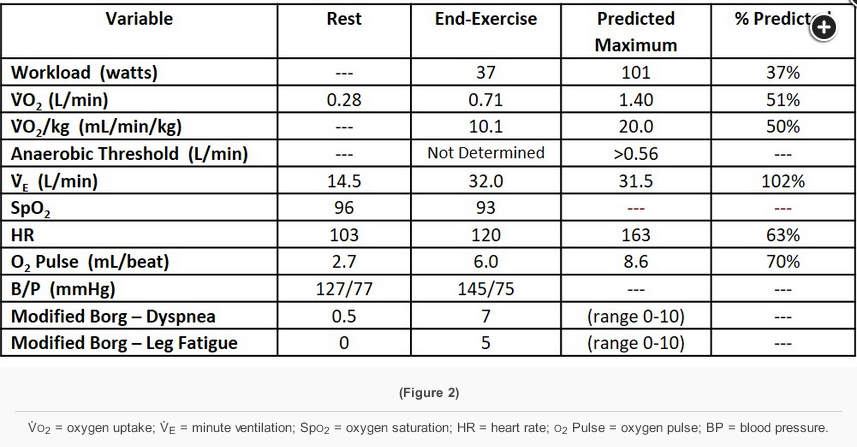
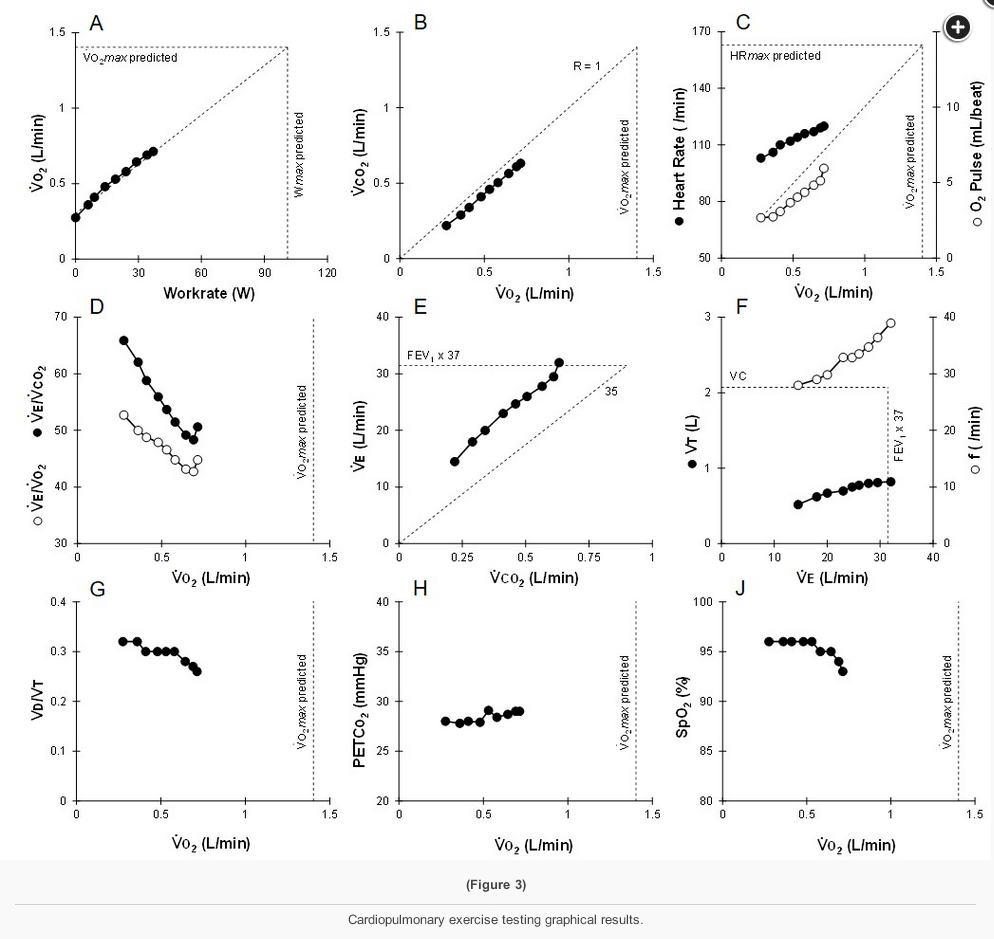
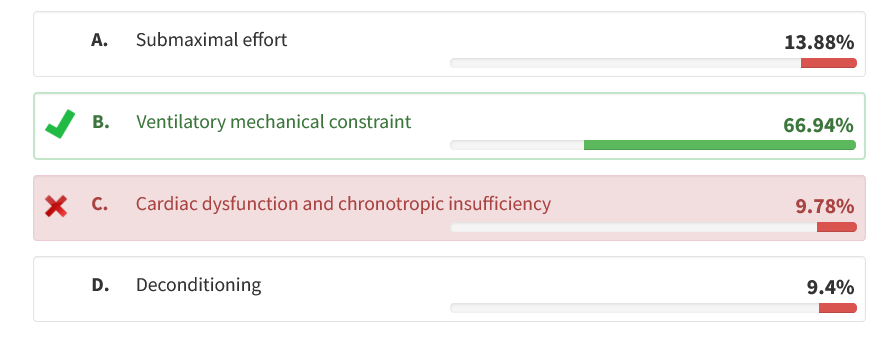
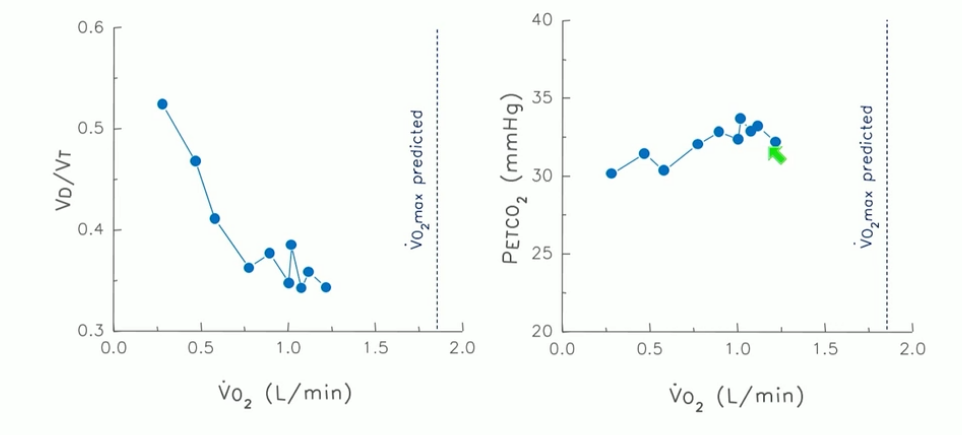
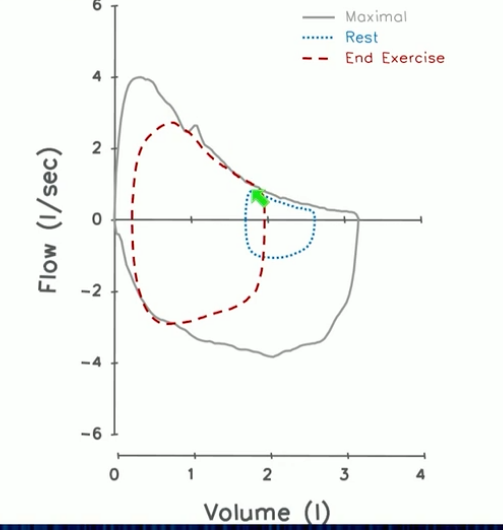
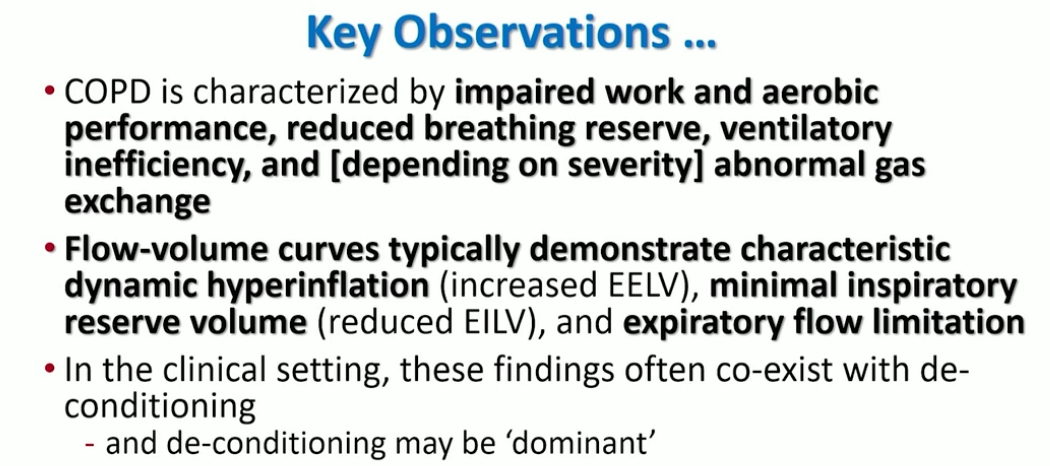
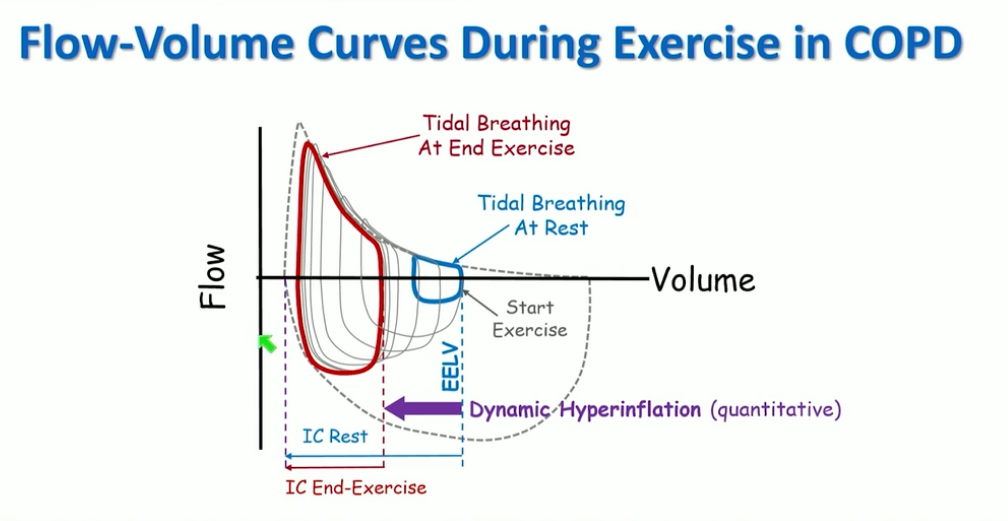
This patient with severe COPD (FEV1 36% predicted) demonstrates marked impairment in work (end-exercise workload 37% predicted) and aerobic capacity (peak V̇o2 51% predicted) that aligns with the clinical history of significant activity limitation (Figure 2). At the end of exercise, the patient had absent breathing reserve and exceeded the predicted maximal ventilation (102% predicted) (Figure 3 [Panel E]). Flow-volume curves during testing demonstrate expiratory flow limitation at rest, during and at end-exercise, with significant dynamic hyperinflation during exercise of ~600 mLs (end-expiratory lung volume [EELV] at rest increases compared with EELV at end-exercise), and near-absent inspiratory reserve volume (IRV) at end-exercise (~160 mLs) (Figure 5). These findings markedly increase the work of breathing and are most consistent with exercise limitation attributable to ventilatory mechanical constraint (choice B is correct).
Submaximal effort may be inferred in the absence of a physiologic maximum having been reached, as maximal exercise in the normal human is characteristically limited by the cardiovascular system. In contrast, this patient reached their predicted maximal ventilation (choice A is incorrect). There were no significant arrhythmias or ischemic changes during exercise, and both the heart rate and O2 pulse were appropriate given the submaximal cardiovascular response during exercise (the patient discontinued exercise because of ventilatory constraint and not the cardiovascular system; choice C is incorrect). Similarly, these findings are not characteristic of deconditioning, although deconditioning is a common finding in many patients with significant COPD (choice D is incorrect). Test results with deconditioning often demonstrate exercise limited by the cardiovascular system but with reduced work and aerobic capacity, an early anaerobic threshold, and an exaggerated heart rate during exercise, unless exercise limitation is associated with a physiologically submaximal effort.
The results from this study suggest that directed efforts to further improving lung function (such as optimizing bronchodilator therapy) would be the most impactful in enhancing exercise performance in this patient. The partial bronchodilator response (10% and 320 mLs) when supported by resting pulmonary function testing may present further opportunity in this regard. Participation in pulmonary rehabilitation and exercise reconditioning would decrease the potential contribution of peripheral muscles to the heightened ventilatory response typical of patients with advanced COPD (Figure 3, panels D and E), thereby also leading to improved exercise performance. Unfortunately, if further augmenting therapy did not lead to improvement in lung function, and/or the patient were already enrolled in an effective pulmonary rehabilitation program, potential gains in activity limitation would be less. Nonetheless, there are other evidence-based reasons to maintain participation in pulmonary rehabilitation, including for the prevention of acute exacerbations, improved quality of life, and maintenance of the current exercise performance.
Case 3
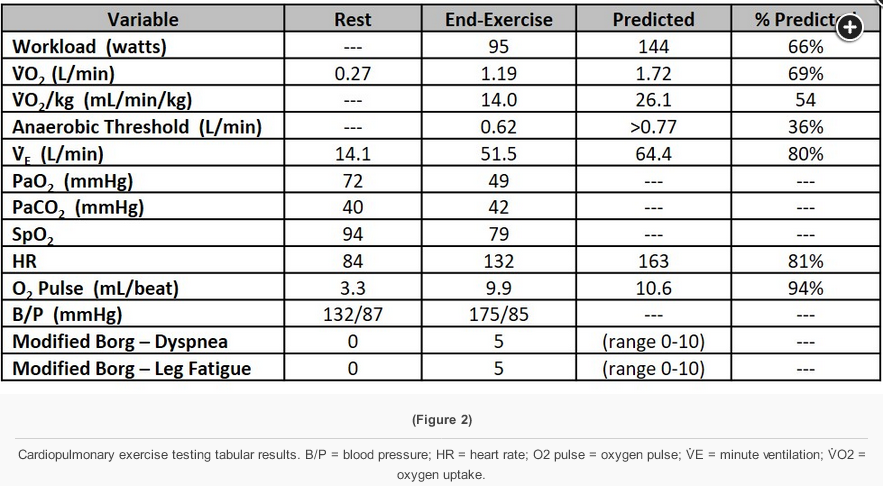
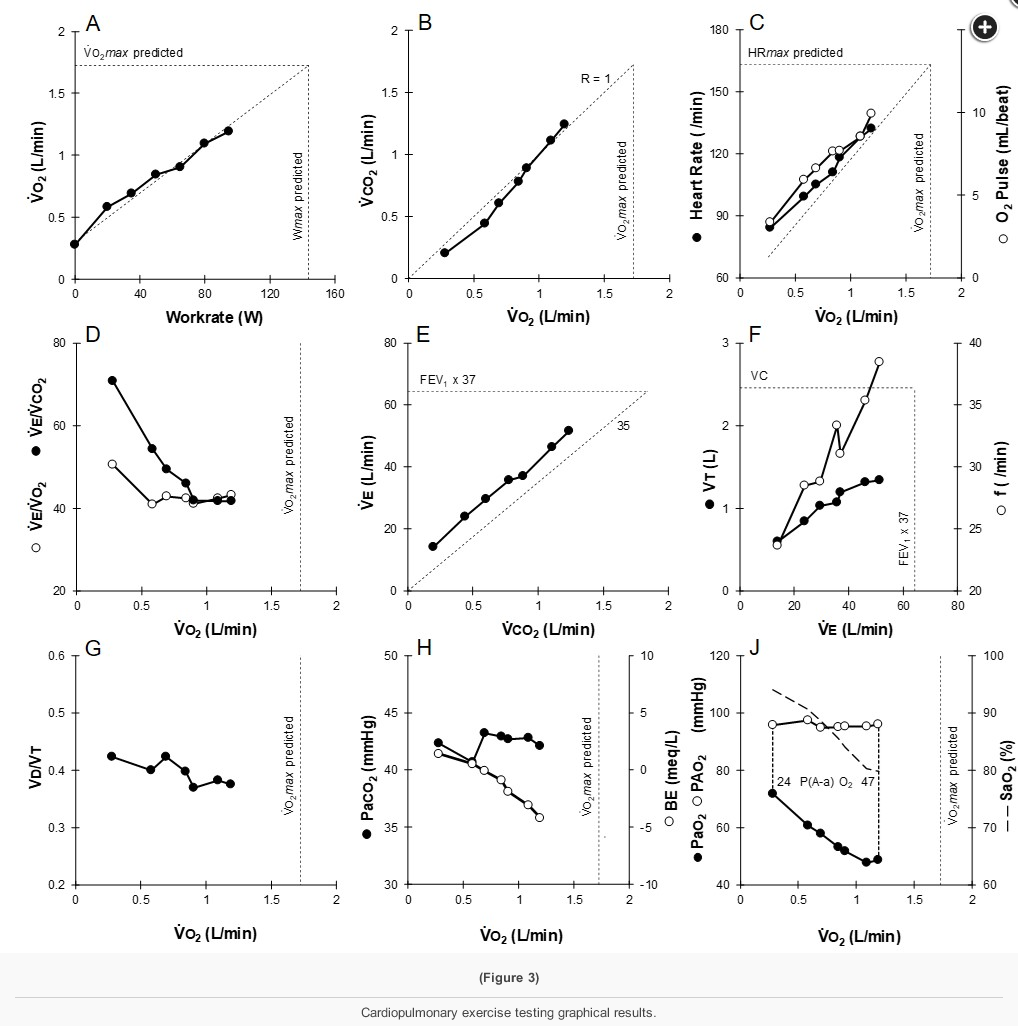
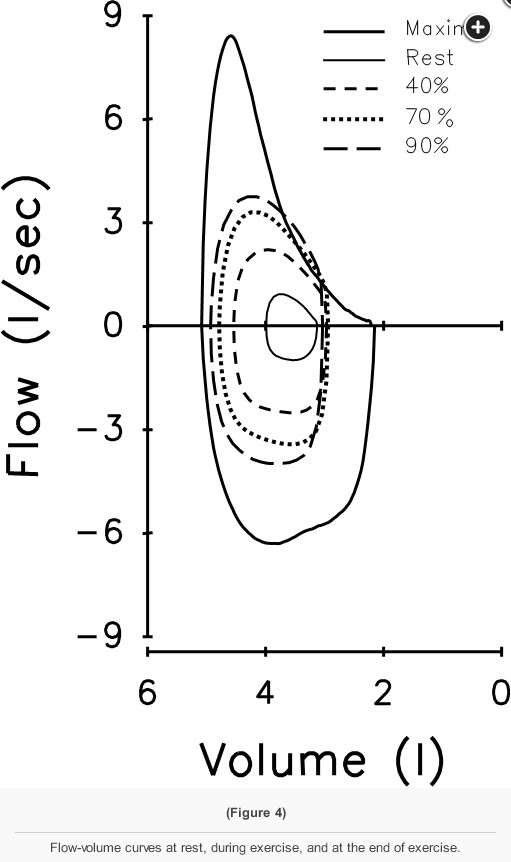
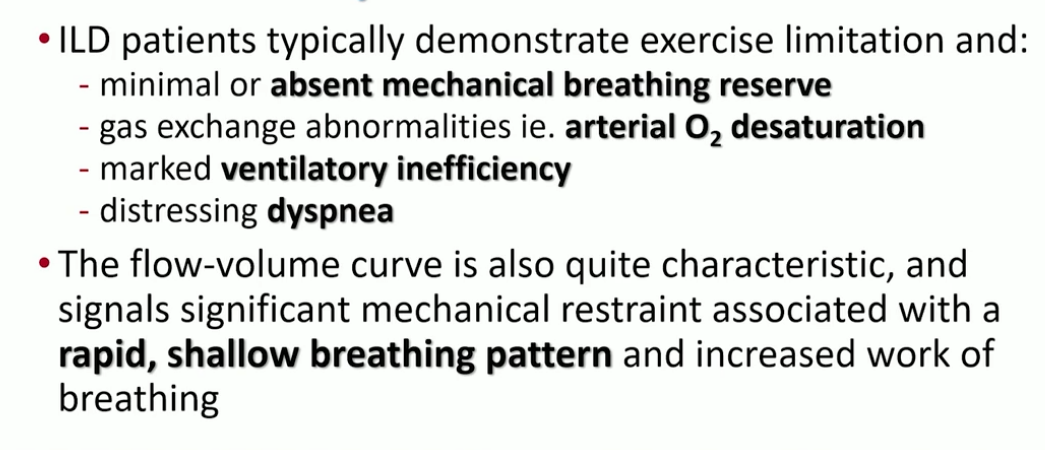
This patient demonstrates significant exercise limitation with a markedly reduced work capacity (end-exercise workload 66% predicted), decreased aerobic capacity (peak V̇O2 69% predicted), and a low anaerobic threshold (36% predicted maximal peak V̇O2) (Figure 2). While estimated maximal ventilatory capacity is not achieved (V̇E /MVV 80% predicted) (Figure 3, panel E, and Figure 4), V̇E is increased during submaximal exercise (Figure 3, panel E), and there are a blunted VT response during exercise (Figure 3, panel F), markedly elevated ventilatory equivalents for both O2 and CO2 (Figure 3, panel D), abnormal gas exchange with desaturation to 79% at the end of exercise, and a widened A-a gradient during exercise (Figure 3, panel J). Inspection of the flow-volume curves (Figure 4) demonstrates near absent inspiratory reserve volume, with minimal reserve to increase tidal volume further. These findings, together with the resting pulmonary function test results, are highly suggestive of interstitial lung disease (ILD) (choice D is correct).
ILD is physiologically characterized by increased elastic loading and decreased static lung compliance, leading to altered ventilatory mechanics manifested in part by a rapid, shallow breathing pattern. In addition, significant V/Q mismatch, diffusion limitation, and reduced mixed venous O2 (SvO2) contribute to impaired gas exchange. In this patient, exercise was limited by markedly abnormal gas exchange before a mechanical ventilatory limitation was achieved. Nonetheless, there is clear evidence of ventilatory inefficiency, an abnormal breathing pattern, and reduced breathing reserve at the end of exercise. Other known contributors to exercise limitation in this population include abnormal pulmonary vasculature and cardiovascular function, as well as compromised peripheral muscle function. These are difficult to assess independently in this instance. However, if exercise were repeated with the patient breathing a hyperoxic inspirate (thus reducing the physiologic manifestations of hypoxemia and decreased O2 delivery), the contribution of these other factors could potentially be better understood.
The reported results from testing seem appropriate in this instance and can therefore be interpreted as outlined—there are no apparent significant technical issues that would preclude interpretation (choice A is incorrect). Although deconditioning is a common finding in patients with exertional dyspnea, they would not display such markedly abnormal ventilatory mechanics and abnormal gas exchange (choice B is incorrect). There is no history of cardiac disease, cardiac examination is normal, and the resting ECG is normal. The lack of a tachycardic heart rate response, the normal oxygen pulse during exercise (although this can be decreased when O2 content is reduced in the setting of significant O2 desaturation or R → L shunt), the lack of other abnormalities consistent with impaired cardiac function, and the presence of characteristic findings of ILD exclude cardiac dysfunction as the etiology most responsible for exercise limitation in this patient (choice C is incorrect).
CHEST cases
- over 90% is normal
- AT: all aerobic to aerobic + anaerobic metabolism
- <40 abnormal
- 40-50: a little low
- 50-55: most of the time
- Ve: 70-80% normal
- BR: 15L or more is normal
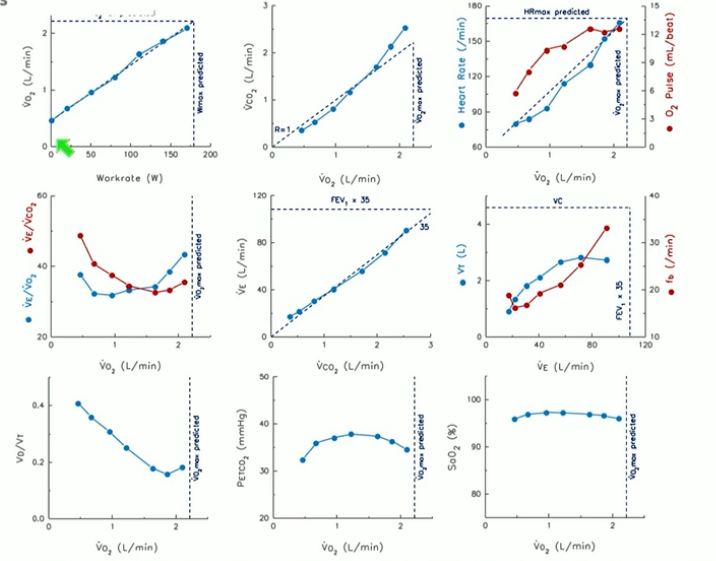
- left: normal
- right: crossing point is indicator for anaerobic threshold
- O2 pulse correlates with stroke volume, if O2 content steady
- right: ventilatory equivalence
- lowest point should be lower than 35. Higher = increased ventilatory response. Breathing more than expected
- lowest point should be lower than 35. Higher = increased ventilatory response. Breathing more than expected
- left
- VCO2 drives ventilation
- 35: is slope
- abnormal: up and shift to left with higher slope
- right: modified hey plot. RR vs TV
- fb: respiratory frequency
- abnormal would be rapid shallow breathing
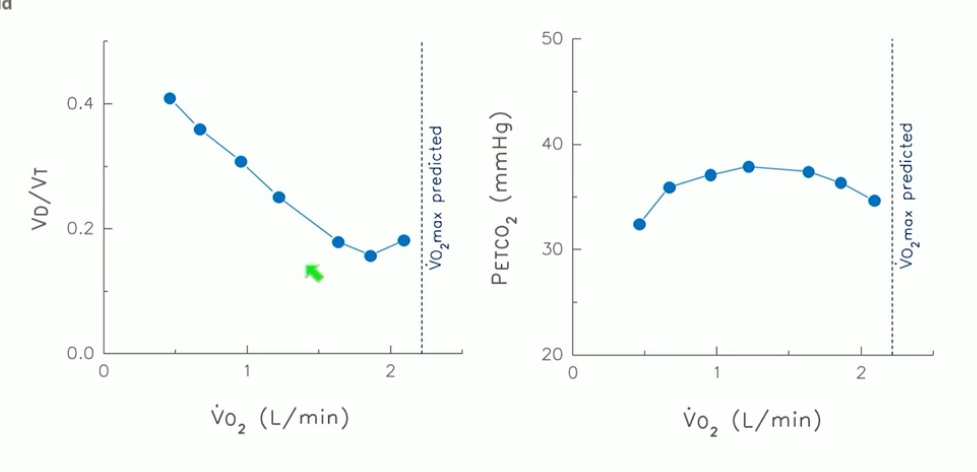
- left: dead space ventilation
- at rest: smallest
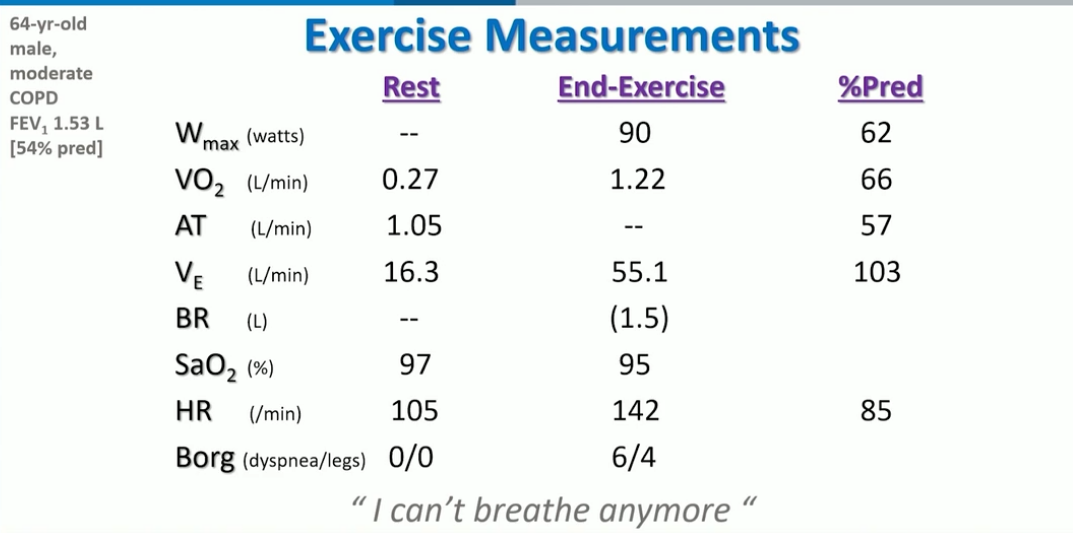
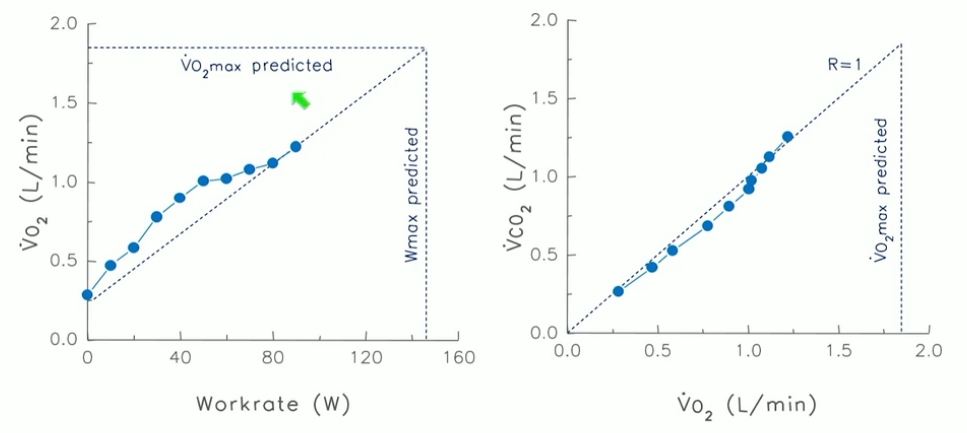
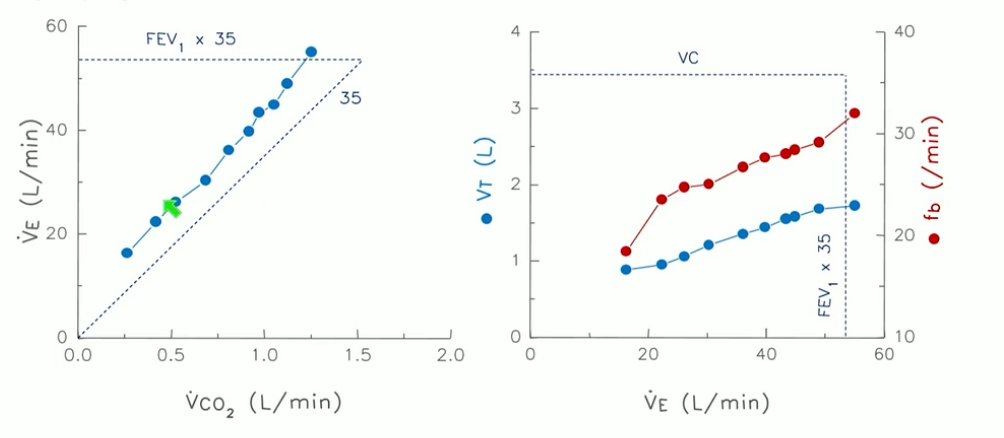
Case 2
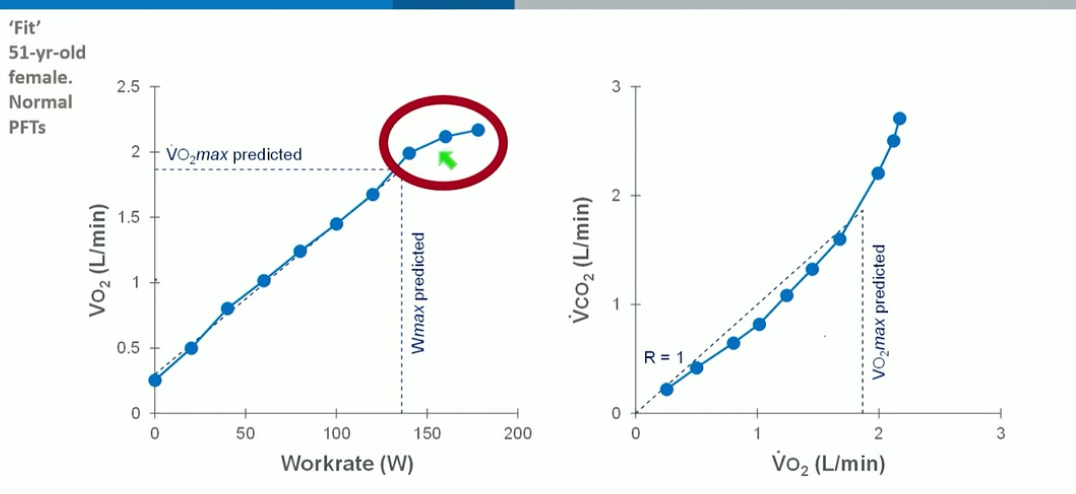
- left: VO2 plateau: gold standard for determining peak VO2
Case 3
- low work and aerobic exercise with normal anaerobic threshold
- reached predicted maximal ventilation without reaching predicted max HR
- Ve: maximal ventilation high with very low breathing reserve
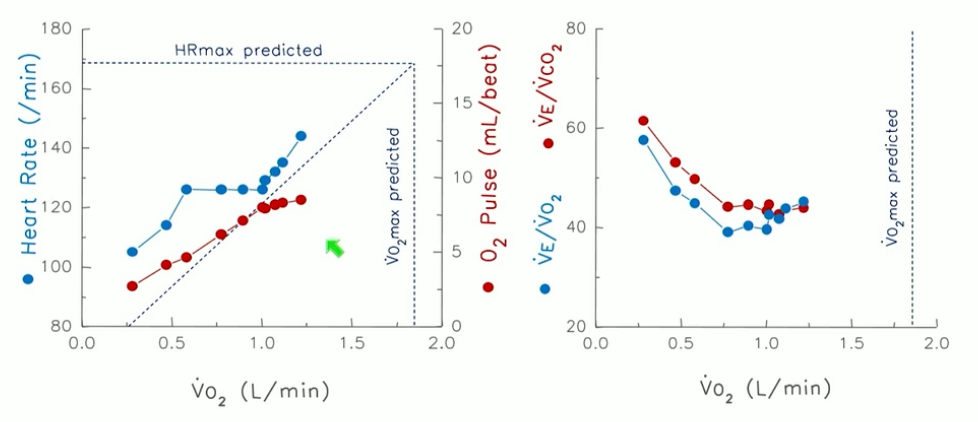
- HR did not reach max
- ventilatory equalvanence nadir is high at 38: increased ventilatory response because of inefficiency
- higher than 35, abnormal
- TV response blunted
- expiratory frequency went up
- very abnormal
- flow limited at rest and at exercise
- end expiratory lung volume changed consistent with dynamic hyperinflation
- can’t breath out
- revisit
- increased Ve/VO2 because of dead space ventilation
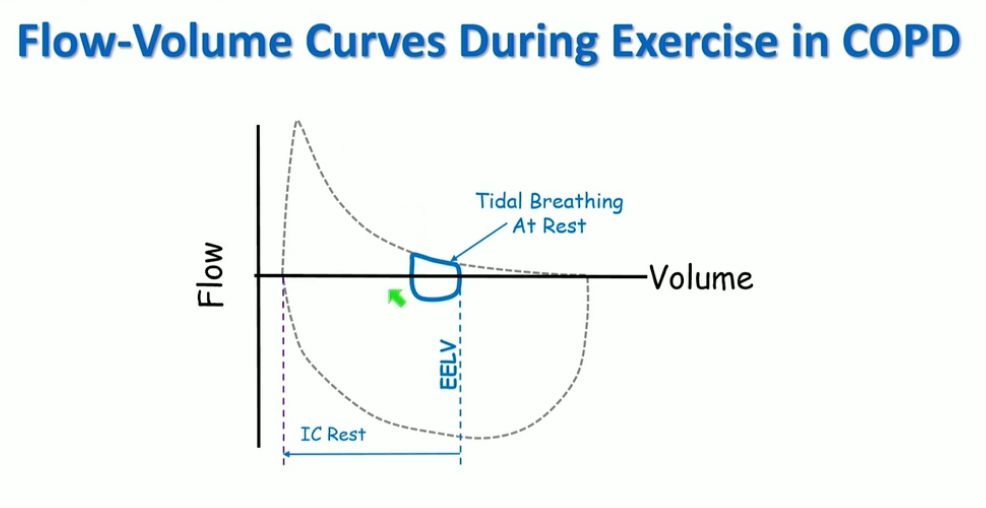
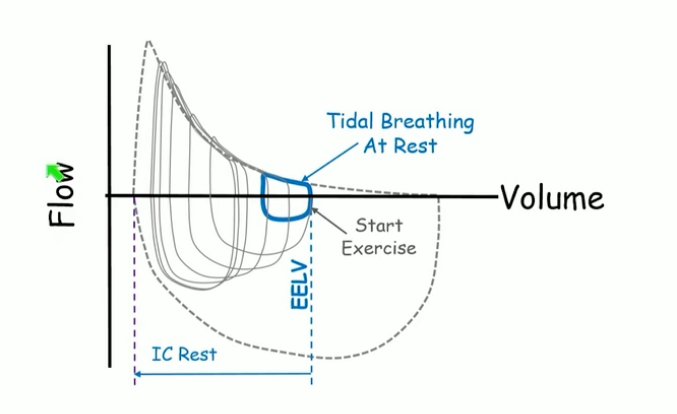
- take bigger breath but can’t breath out
- with exercise, every breath is almost biggest breath you can take
- work of breathing increases
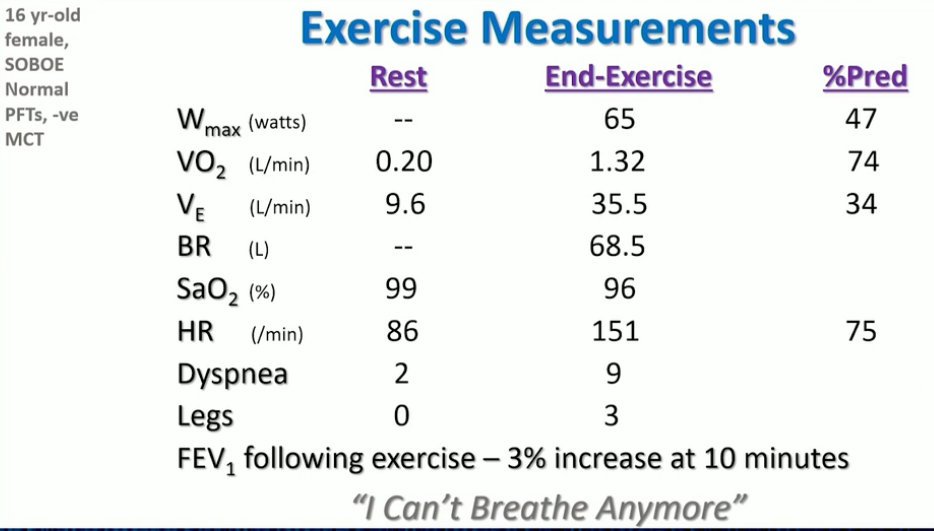
Case 4
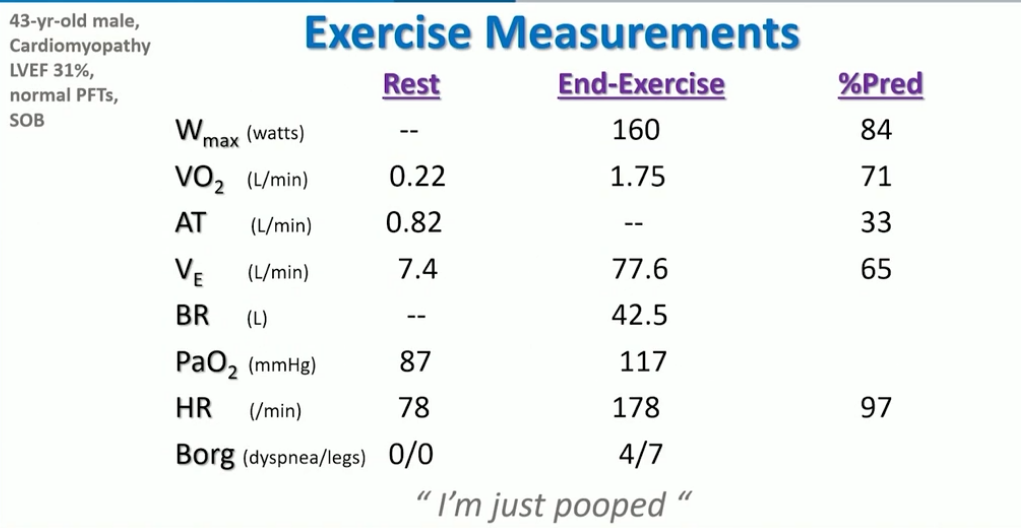
- a little low max work rate and VO2
- AT reduced: early AT
- lots of breathing reserve
- A line shows increased O2 at end of exercise
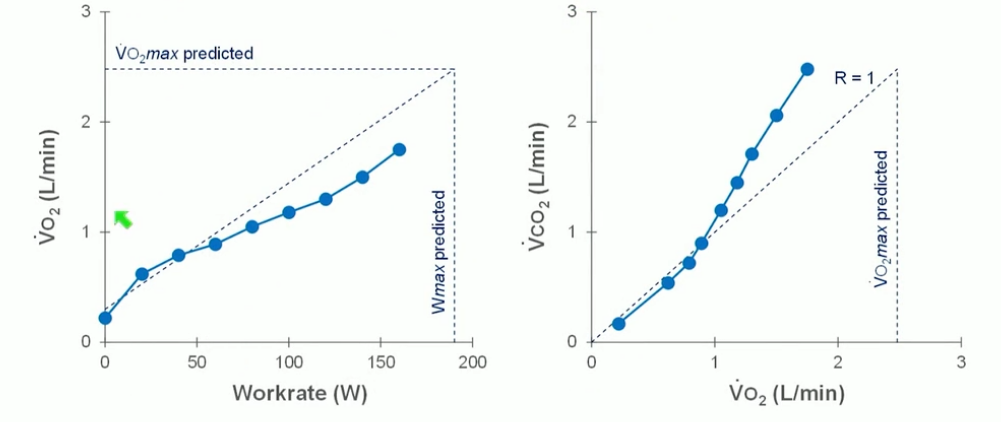
- left: down and to right characteristics of CV abnormality
- right: early AT with slope change
- SV plateaus early and HR goes up early
- normal ventilatory equivalence
- MV normal
- breathing response normal
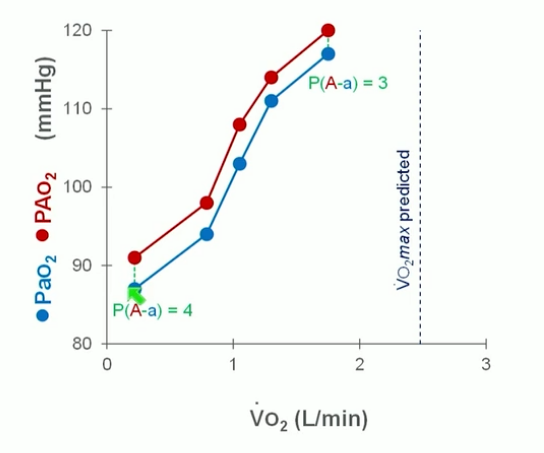
- Aa gradient normal
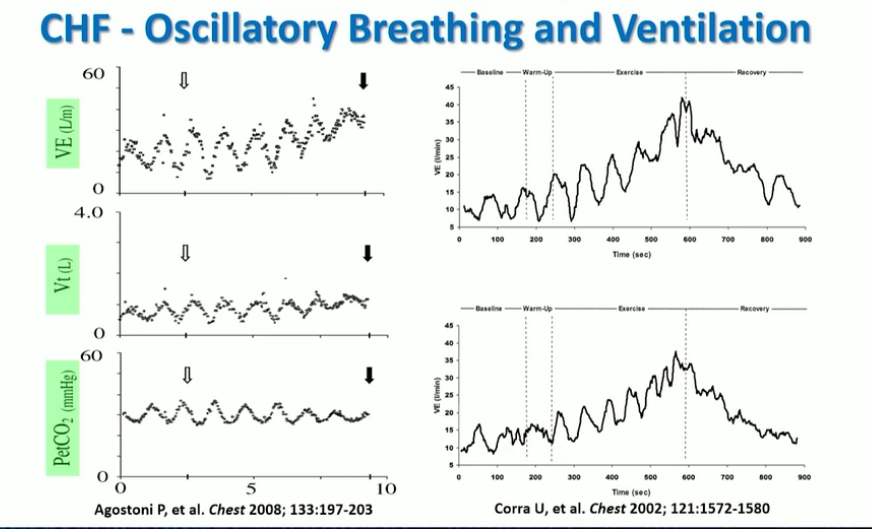
- like Cheynne stokes but not exactly
- cyclical rhythmic
- see this, pick heart failure
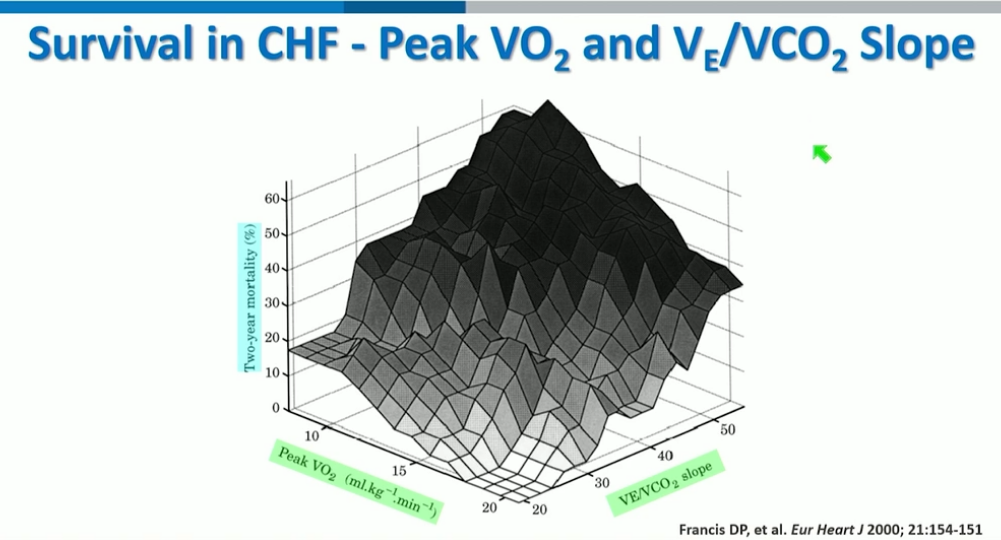
- 2 most important factors for outcome in heart failure
Case 5
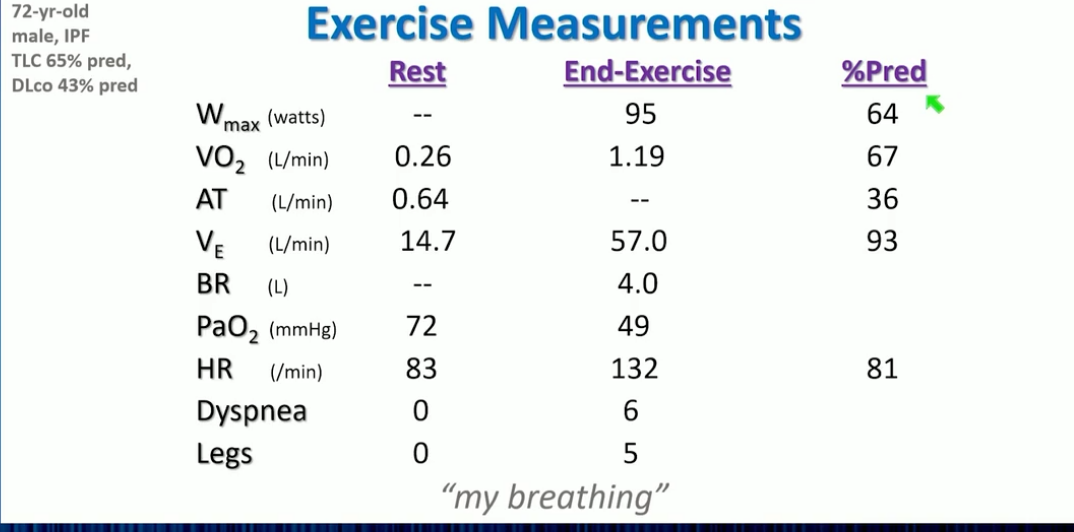
- high decrease in PO2
- did not reach max HR because can’t breath and desatted
- early anaerobic threshold
- lots of reserve in CV system
- ventilatory equivalence higher than 40 probably because of AT, deadspace, hypoxemia. Not U shaped because not able to breath anymore
- left: slope is up
- right: blunted TV response
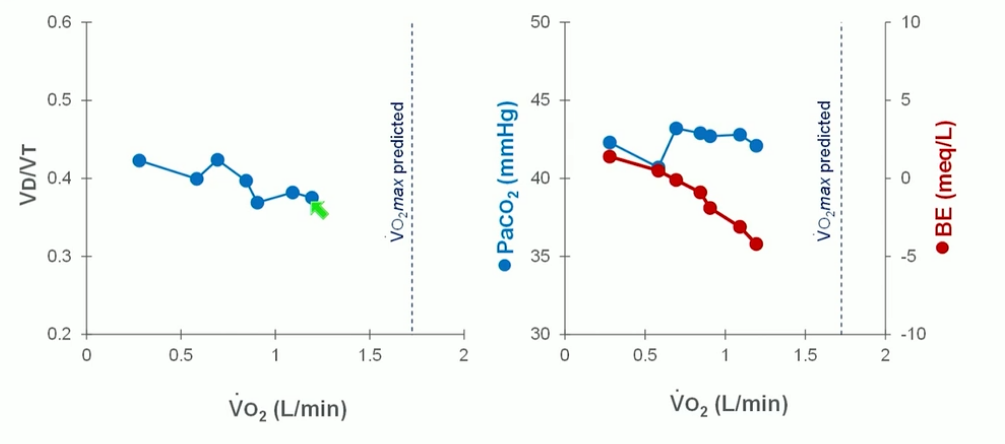
- dead space ventilation is high
- paCO2 did not go down, less base excess = acidotic
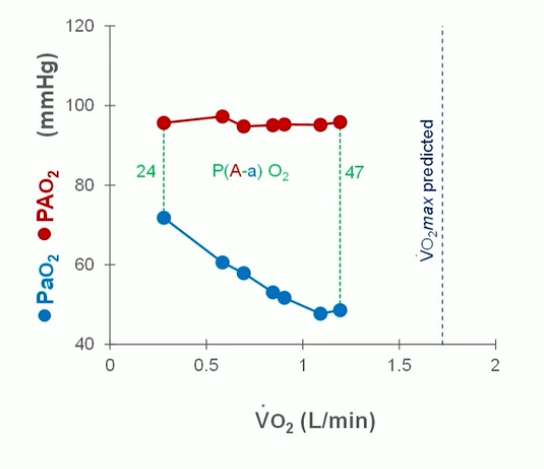
- aa gradient elevated
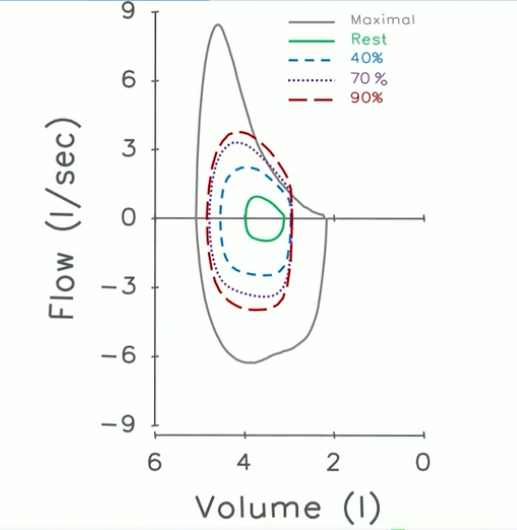
- rapid, fast, everything is constricted
Case 6
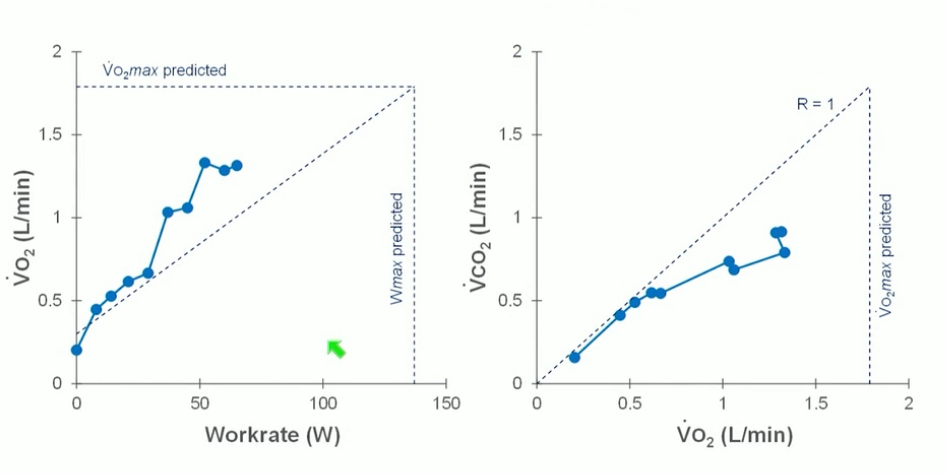
- VO2 moving all over the place
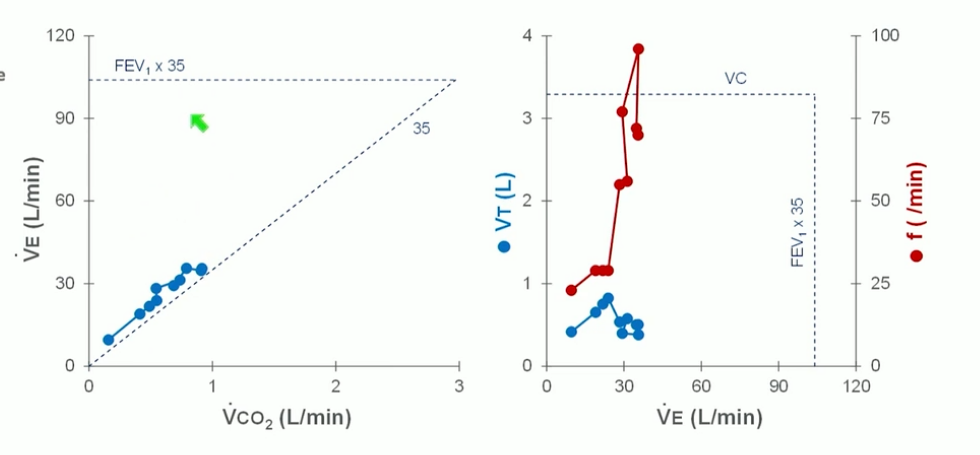
- a lot of ventilatory reserve
- VT low, tachypnea significant
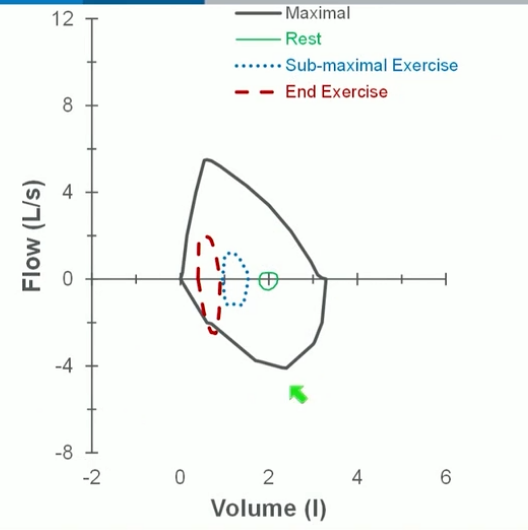
- person chose to dynamically inflate
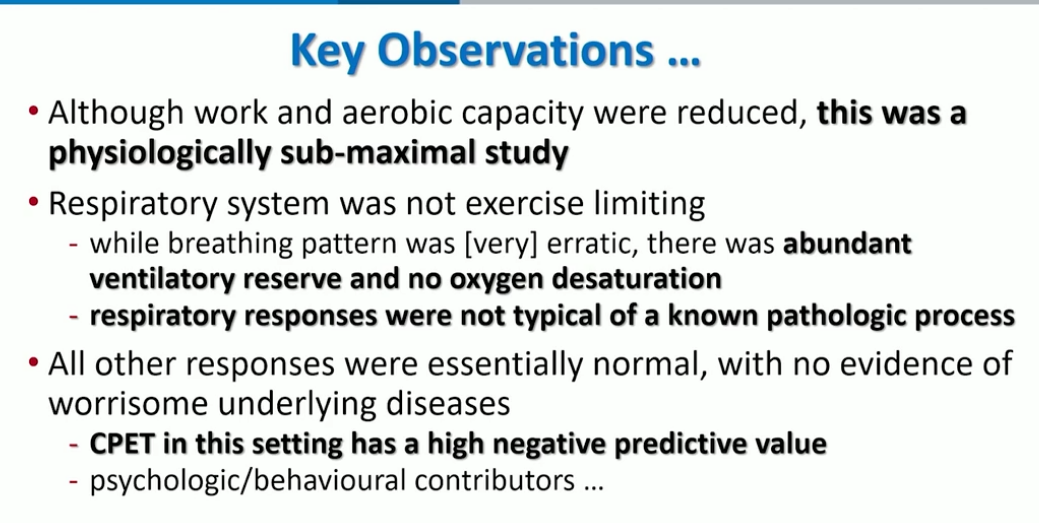
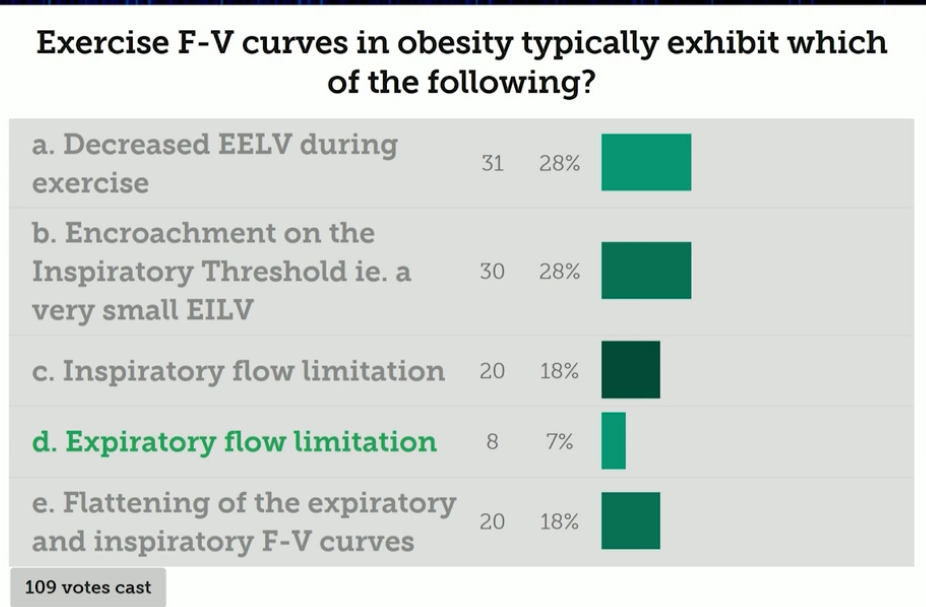
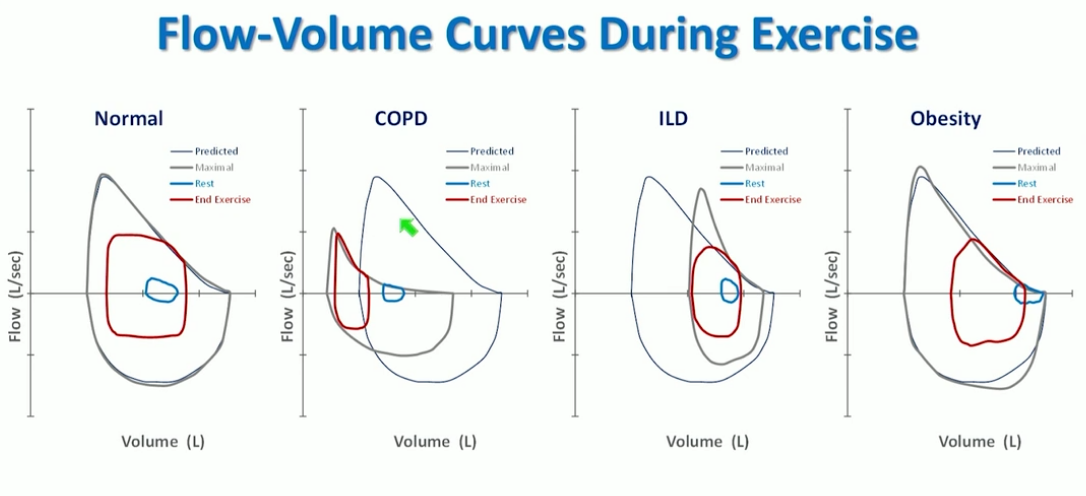
- obesity and normal are very similar except for tidal breathing at rest
- obese person are breathing near RV, flow limited at rest because of mechanics. ERV and FRC very reduced.
- traumatic accident with intubation