selection criteria for lung transplantation in COPD patients
- related: COPD chronic obstructive pulmonary disease
- tags: #permanent
The decision to refer should depend on the patient’s life expectancy, quality of life, and patient preferences. In general, patients at high risk of dying in less than 2 years who have a high probability of 90-day postoperative survival are candidates. Patients with an elevated BODE index (5 or 6), resting hypoxemia, hypercapnia, an FEV1 of less than 25% of predicted, or significant exercise limitation despite medical therapy, smoking cessation, and participation in a pulmonary rehabilitation program may be referred for evaluation for lung transplantation. Transplantation improves quality of life, and the median life expectancy is 5.7 years.
This patient has discontinued tobacco use for >6 months, is on optimal medical therapy, and is participating in rehabilitation, yet she continues to experience severe dyspnea and is dissatisfied with her quality of life. Carefully selected patients with advanced COPD and continued dyspnea may benefit from procedures such as lung volume reduction surgery (LVRS), bronchoscopic lung volume reduction (LVR) using endobronchial valves (EBV) or other techniques, or lung transplantation (LT). This patient is best suited for LT referral.
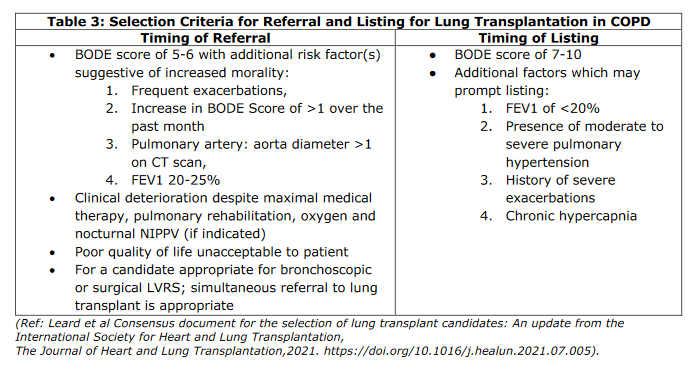
Criteria for LT for COPD in consensus-based guidelines are based on the balance between need and benefit and include progressive disease despite maximal treatment with medication, pulmonary rehabilitation, and oxygen therapy. In addition, the patient should not be a candidate for LVRS or bronchoscopic LVR (in selected cases, both referrals can be placed concurrently). For referral for LT evaluation, patients should have a BODE (body mass index, degree of airflow obstruction, dyspnea, and exercise capacity) score of 5 to 6 and one or more of the following: postbronchodilator FEV1 of 20% to 25% predicted, increasing BODE score over the past 24 months, frequent exacerbations, or pulmonary-artery-to-aorta diameter >1 on CT scan; clinical deterioration despite appropriate therapy; or poor quality of life unacceptable to the patient. Listing criteria for LT includes one or more of the following: BODE score of 7 to 10, FEV1 of <20% predicted; moderate to severe pulmonary hypertension; history of severe exacerbations; and chronic hypercapnia. Evidence suggests that functional capacity and quality of life are improved following LT for COPD, and some data suggest a survival advantage. General LT criteria also include age <70 years and BMI between 16 and 35 kg/m2.
LVRS surgically removes an area of emphysematous lung with the goals of reducing hyperinflation and allowing better function of the remaining lung. A large trial of surgical LVRS vs maximal medical therapy showed a survival advantage in the group of patients with heterogeneous upper lobe emphysema and low exercise capacity after at least 6 weeks of rehabilitation; the latter was defined as 25 W for women and 40 W for men. Poor outcomes and an increase in mortality occurred in patients with an FEV1 of <20% predicted and either DLCO of <20% predicted or non-upper-lobe emphysema (homogeneous) on chest CT scan. This patient does not meet criteria for LVRS and in fact has many of the contraindications, including severity of pulmonary function test results, homogeneous emphysema, and severity of gas exchange; therefore, she should not undergo evaluation for LVRS (choice B is incorrect).
Newer techniques of bronchoscopic LVR also exist. These interventions allow placement of devices such as endobronchial one-way valves, plugs, blockers, coils, or stents or thermal airway ablation in the most emphysematous and diseased areas of the lungs to result in atelectasis and essentially eliminate the targeted area of lung. One major difference between LVRS and bronchoscopic LVR is that select patients with homogeneous emphysema can be considered for bronchoscopic LVR if there is a complete fissure based on specialized high-resolution CT or other analysis and little or no collateral ventilation in the target lobe in which the EBV will be placed, but these patients must have significant hyperinflation and air trapping. Two types of EBV are approved in the United States, and these interventions are part of the GOLD guidelines. EBV insertion in selected patients with advanced COPD has been shown to provide improvement in lung function (FEV1, RV, and RV/TLC), exercise tolerance (6-min walk test), dyspnea (improved MMRC score), and quality of life (St. George’s Respiratory Questionnaire score) at 12 months. EBV insertion has not been shown to reduce all-cause mortality. Pneumothoraces are a common complication of these procedures and occur in 25% to 29% of cases. Acute exacerbation of COPD and deaths have also been described. Importantly, placement of EBVs does not preclude subsequent LVRS or LT. Absolute contraindications to EBV placement include the absence of a complete fissure, elevated PAPs (usually PASP >50 mm Hg), DLCO <20% predicted, FEV1 <15% predicted, significant hypoxemia <45 mm Hg at rest on room air, hypercapnia >60 mm Hg, heart disease with LVEF <45%, and active and recurrent exacerbations and pulmonary infection. Strong relative contraindications include the absence of hyperinflation (eg, postbronchodilator RV <150%-175% predicted by body plethysmography and RV/TLC <55%). Many of these contraindications are present in this patient (choice C is incorrect). In addition, the degree of air trapping in this patient is less than in those usually benefiting from EBV placement; ideally selected patients would have RV >150% to 175% predicted and RV/TLC ≥55%.
Although palliative care and goals of care (GOC) discussions and symptom management for dyspnea, cough, sputum production, weakness, anxiety and depression, and pain are appropriate, this patient has not expressed interest in hospice care (generally reserved for terminal illness with <6 months’ life expectancy and when GOC are aligned). Hospice referral at this time would not be appropriate given the patient’s desire to “try everything” even though palliative care referral for symptom management and GOC discussions could be appropriate (choice D is incorrect).2
Links to this note
Footnotes
-
COPD Part III LVRS, Bipap, and Transplant ↩