serotonin syndrome
- related: Neurology
- tags: #literature #icu #neuro
This patient has developed serotonin toxicity, or serotonin syndrome. Serotonin syndrome results from increased serotonergic activity in the CNS and can be life-threatening. The diagnosis is made clinically but should be considered in patients with spontaneous clonus, inducible clonus with agitation, ocular clonus, or tremor and hyperreflexia. Other clinical features of serotonin syndrome include restlessness, hyperreflexia, muscle rigidity, myoclonus, dilated pupils, flushed skin, increased bowel sounds, bilateral Babinski signs, and dry mucous membranes. Hyperreflexia and clonus are particularly common and are more pronounced in the lower extremities. Serotonin syndrome can occur with therapeutic selective serotonin reuptake inhibitor (SSRI) use or inadvertent interactions between drugs. Infection increases the risk of developing serotonin syndrome. In this patient, the addition of methylene blue to sertraline is the likely etiology. Other potential drugs that interact with SSRIs and can cause serotonin toxicity include fentanyl, linezolid, procarbazine, and other monoamine oxidase inhibitors. Most cases of serotonin syndrome present within 6 h, and almost all within 24 h, of a change in dose or initiation of a drug.
Treatment involves supportive care and cessation of the serotonergic agent. Agitation and neuromuscular abnormalities should be treated with benzodiazepines and cyproheptadine, a nonspecific serotonin antagonist (choice D is correct). In cases with profound hyperthermia (temperature >41°C), patients should also be treated with sedation, endotracheal intubation, and paralysis.
Hyperthermia is also seen with malignant hyperthermia in response to inhaled anesthetics or neuromuscular blockers like succinylcholine. While she likely received some of these agents in the operating room the day before, malignant hyperthermia almost always manifests in the operating room or immediately postoperatively. Although cases have been reported up to 48 to 72 h after exposure, this is very unusual. While malignant hyperthermia shares some signs and symptoms with serotonin syndrome, such as hyperthermia and muscle rigidity, malignant hyperthermia does not induce clonus, skin flushing, or hyperactive bowel sounds. Dantrolene, the treatment of choice for malignant hyperthermia, is not useful in the treatment of serotonin toxicity (choice C is incorrect).
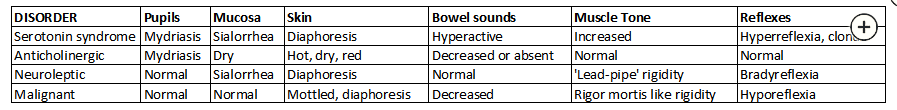
Neuroleptic malignant syndrome and anticholinergic toxidromes are also in the differential diagnosis. However, this patient has no known exposures to antipsychotics, making neuroleptic malignant syndrome unlikely. In addition, neuroleptic malignant syndrome does not cause hyperactive bowel sounds or hyperreflexia and clonus. Anticholinergic toxidromes have dry skin and mucous membranes. Unlike this patient, those with anticholinergic toxidromes have hypoactive bowel sounds and normoreflexia. The table lists distinguishing features of the syndromes under consideration for this patient (Figure 1).
A 64-year-old woman with a history of cirrhosis from nonalcoholic steatohepatitis complicated by hepatic encephalopathy and esophageal varices, depression treated with sertraline, and type 2 diabetes mellitus fell at home and fractured the femoral neck of her left hip. Following hip arthroplasty, she is admitted to the ICU due to persistent hypotension. Her BP is 95/46 mm Hg on low-dose norepinephrine and heart rate is 96/min, and she is resting comfortably in bed on room air, breathing 18/min. She is slightly confused but easily redirectable. Diagnostic paracentesis shows no evidence of peritonitis, but she is given empirical ceftazidime and vancomycin. The next morning, she remains on low-dose norepinephrine, with no change in BP. Methylene blue is given intravenously for vasoplegia.
Later in the morning, you are called for worsening hypotension and disorientation. Vital signs are a temperature of 38.9°C, heart rate of 124/min (irregularly irregular), and BP of 88/35 mm Hg on high-dose norepinephrine and vasopressin. She is breathing 28/min and is diaphoretic and responsive but very confused and disoriented. The abdominal exam is notable for hyperactive bowel sounds but is soft, nontender, and slightly distended with a fluid wave. All four extremities show rigidity and hyperreflexia, with spontaneous clonus in both ankles and upward moving toes on stimulation of the soles. Compared with earlier in the morning, serum bicarbonate has fallen from 22 to 13 mEq/L (22 to 13 mmol/L), creatinine has risen from 0.7 to 1.6 mg/dL (61.88 to 141.44 μmol/L), and the international normalized ratio is higher (1.6 to 3.1). Creatine kinase is 15,416 (40-150) U/L (257.45 [0.67-2.50] μkat/L), and lactic acid is 11.4 (0.5-2.0) mg/dL (1.27 [0.06-0.22] mmol/L).
What is the best next treatment in the management of her condition?