small ETT can cause secretion accumulation
- related: ICU intensive care unit
- tags: #literature #icu
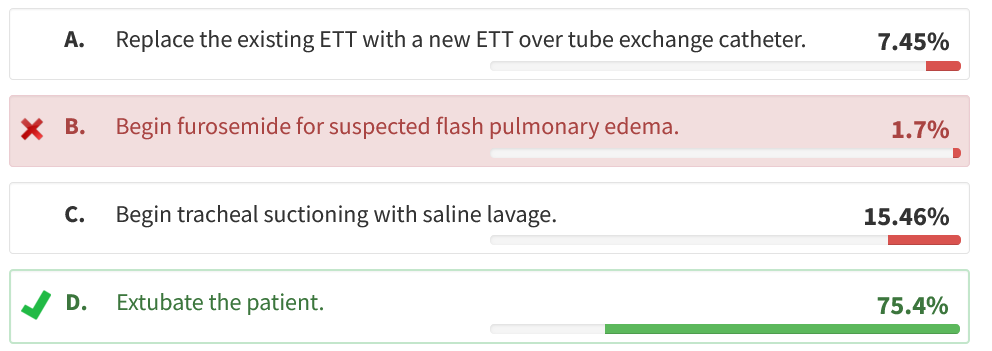
This patient has a clinical picture strongly suggestive of severe narrowing of the lumen of the ETT as a result of accumulation of secretions (Figure 1). Among the options, proceeding to extubation would be most appropriate.
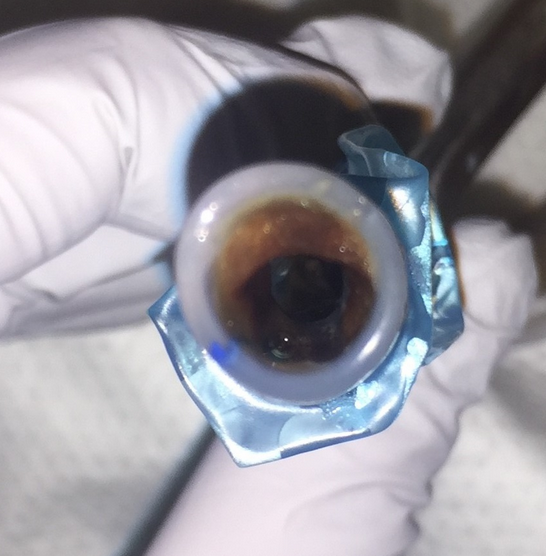
Accumulation of secretions on the inner surface of the ETT is common and can become so severe as to compromise the effective inside diameter of the ETT. In one series, the average depth of debris was 0.64 mm and average thickest accumulation was 2.0 mm. The resulting effective inside diameter can decrease to 4 mm, the outside diameter of the in-line suction catheter. Resistance to passing the suction catheter is typically present. Given that airflow resistance is proportional to the 4th power of the radius, such narrowing produces significant added work of breathing, particularly during efforts with more rapid airflow, such as during a spontaneous breathing trial. Additionally, residual bronchial secretions can migrate to the ETT, such as during a cough, and further narrow or even completely occlude the already narrowed ETT lumen—a potentially life-threatening event.
Narrowing of the ETT lumen is an important cause of increased peak airway pressure (Ppeak), triggering the high pressure alarm. In the stable patient receiving volume control ventilation, an important step in investigating the cause of the elevated Ppeak is to measure plateau pressure (Pplat) by pausing airflow at end inspiration, allowing pressure within the patient-airway circuit to equilibrate at end inspiration (so called inspiratory pause or inspiratory hold). If high Ppeak is caused by increased airway resistance, the Pplat should be normal and the Ppeak-Pplat difference > 8 to 10 cm H2O. Common causes of acutely increased airway resistance include narrowing of the ETT due to accumulation of secretions, kinking, or patient biting and bronchospasm or bronchial secretions. In contrast, the presence of high Ppeak accompanied by high Pplat with a difference of <5 cm H2O indicates a problem with reduced thoracic compliance. Common conditions that acutely reduce compliance include ETT tip position within a mainstem bronchi, pulmonary edema, pneumonia (aspiration), large atelectasis, pulmonary hyperinflation, pneumothorax, large pleural fluid/blood collection, and abdominal distension or reduced chest wall compliance. In our case, Pplat is normal and the Ppeak-Pplat difference is > 10 cm H2O, consistent with increased airway resistance such as that caused by accumulation of secretions in the ETT. The findings are not consistent with reduced pulmonary compliance, making flash pulmonary edema unlikely.
Management of significant accumulation of secretions within the ETT can be challenging. Performing traditional in-line suctioning only transiently reestablishes a patent ETT in those who have distress related to narrowing. Instillation of normal saline before suctioning does not improve secretion clearance from ETT or bronchi and, according to meta-analysis of randomized controlled trials, is more likely to cause a fall in oxygen saturation.
A number of devices designed to be inserted into the ETT and scrape the secretions off the luminal surface of the ETT have been demonstrated to remove secretions and modestly reduce airway resistance. These devices hold promise but are not yet widely used. Accumulation of secretions within the ETT can delay successful extubation, worsen work of breathing, and progress to life-threatening airway occlusion. Accordingly, the ETT should be removed. Features of this case indicate a high likelihood of successful extubation, because the patient has passed all other components of the liberation protocol and has overall clinical improvement.
The clinician should prepare for reintubation if necessary and consider extubation to noninvasive ventilation. In contrast, exchanging the current ETT over a tube exchange catheter to a fresh ETT could be hazardous, because the preexisting ETT narrowing would prohibit ventilation while the exchange catheter is within the existing ETT, and ETT removal over the catheter would likely be difficult because of the narrow functional lumen. If the patient were at high risk of experiencing extubation failure, ETT removal and reintubation under direct visualization would be preferred.123456
A 65-year-old man with chronic bronchitis is recovering from acute respiratory failure from pneumonia. He was intubated with a 7.5-mm endotracheal tube (ETT) 1 week ago, and for the past several days his high peak airway pressure alarm has been intermittently activated. Peak airway pressure and plateau pressure are 40 cm H2O and 20 cm H2O, respectively, during one of these events (increased from 30 cm H2O and 20 cm H2O between events). He is anxious and dyspneic but alert and cooperative during the events. He is currently receiving volume control ventilation with the following settings: f = 12/min, tidal volume = 450 mL, PEEP = 5 cm H2O, FiO2 = 0.4. For several days he has passed his ventilator liberation protocol entirely, except that he develops respiratory distress within 30 min of starting the spontaneous breathing trial with pressure support of 5 cm H2O.
The findings of an ECG obtained during a spontaneous breathing trial are unremarkable other than sinus tachycardia (115/min). He is observed to be alert and interactive and has a strong cough productive of small amounts of thick secretions. On examination, his heart rate is 85/min; respiratory rate, 16/min; BP, 140/90 mm Hg; and SpO2, 95%. He is afebrile, has trace pretibial edema, and has rhonchi and a few crackles on lung examination. The in-line suction catheter is passed with some difficulty, and suctioning produces scant thick secretions. A chest radiograph reveals ETT in good position, mild bibasilar atelectasis, and small left lower lobe infiltrate at site of pneumonia. Arterial blood gas measurements include a pH of 7.38, a PCO2 of 55 mm Hg, and a PO2 of 80 mm Hg.
Which of the following interventions would be most appropriate at this time?
Links to this note
Footnotes
-
Coppadoro A, Bellani G, Bronco A, et al. The use of a novel cleaning closed suction system reduces the volume of secretions within the endotracheal tube as assessed by micro-computed tomography: a randomized clinical trial. Ann Intensive Care. 2015;5(1):57. PubMed ↩
-
Covert T, Niu NT. Differential diagnosis of high peak airway pressures. Dimens Crit Care Nurs. 2015;34(1):19-23. PubMed ↩
-
Glass C, Grap MJ, Sessler CN. Endotracheal tube narrowing after closed-system suctioning: prevalence and risk factors. Am J Crit Care. 1999;8(2):93-100. PubMed ↩
-
Tobin MJ. Advances in mechanical ventilation. N Engl J Med. 2001;344(26):1986-1996. PubMed ↩
-
Wang CH, Tsai JC, Chen SF, et al. Normal saline instillation before suctioning: a meta-analysis of randomized controlled trials. Aust Crit Care. 2017;30(5):260-265. PubMed ↩