solitary fibrous tumor of pleura SFTP is benign mobile pleural tumor
- related: lung mass and cancer
- tags: #literature #pulmonology
The radiographic and the histologic findings are consistent with the diagnosis of solitary fibrous tumor of the pleura (SFTP) (choice A is correct). SFTP are tumors of mesenchymal origin and represent less than 5% of pleural masses. SFTP tend to affect adults during the sixth and seventh decades of life and typically present as incidental asymptomatic masses. Larger tumors are generally more likely to present with symptoms while smaller tumors are more commonly asymptomatic. Respiratory symptoms may occur in one-third of patients and can include cough, dyspnea, pleuritic chest pain, and hemoptysis due to compression of a bronchus. Extrathoracic symptoms include hypoglycemia (5% of patients)—related to insulin-like growth factors produced by these tumors—and hypertrophic osteoarthropathy (up to 20% of patients), thought to be related to increased production of hyaluronic acid by tumor cells.
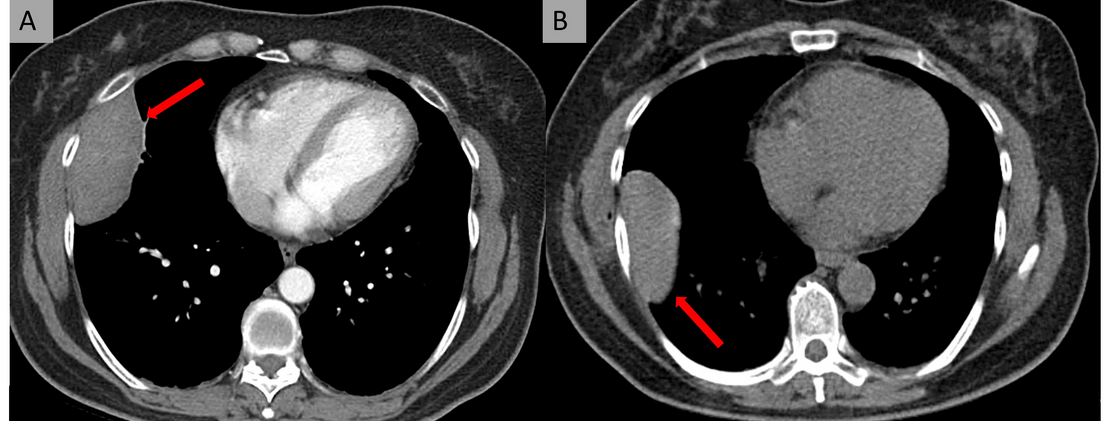
- Two scans highlighting the mobile nature of a SFTP. Figure A: Contrast-enhanced CT. Figure B: Noncontrast-enhanced CT acquired during pertunaneous biopsy.
SFTP are often incidentally found on plain chest radiography or CT. However, the appearance on plain chest radiography is nonspecific and should prompt further investigation. Chest CT is considered the key initial diagnostic modality that can accurately visualize the extent of tumor, its location, and assist in surgical evaluation. The most common imaging appearance is a solitary well-circumscribed lobulated mass that usually arises from the visceral pleura and may be mobile if pedunculated. Evaluation of the two CT scans provided in this case highlight the uniquely characteristic mobile feature of this tumor (Figure 5).
The diagnosis of SFTP can be confirmed only through histopathological analysis. Histologically, hypocellular SFTP are characterized by a dense collagenous background, often with hyalinized or thick collagen bands. Variably atypical spindled cells are arrayed haphazardly within this stroma, in a storiform configuration or in randomly oriented fascicles, often characterized as a “patternless pattern” (Figure 4). Immunohistochemical (IHC) analysis is vital as it can help differentiate SFTP from other spindle cell tumors of the pleura. IHC markers useful in confirming the diagnosis of SFTP include CD34, BCL2, CD99, and vimentin in the absence of actin, desmin, S100 protein, or epithelial markers. Our patient’s specimen was CD34 and BCL2 positive, actin and S-100 negative, and keratin and AE1/AE3 were focally positive.
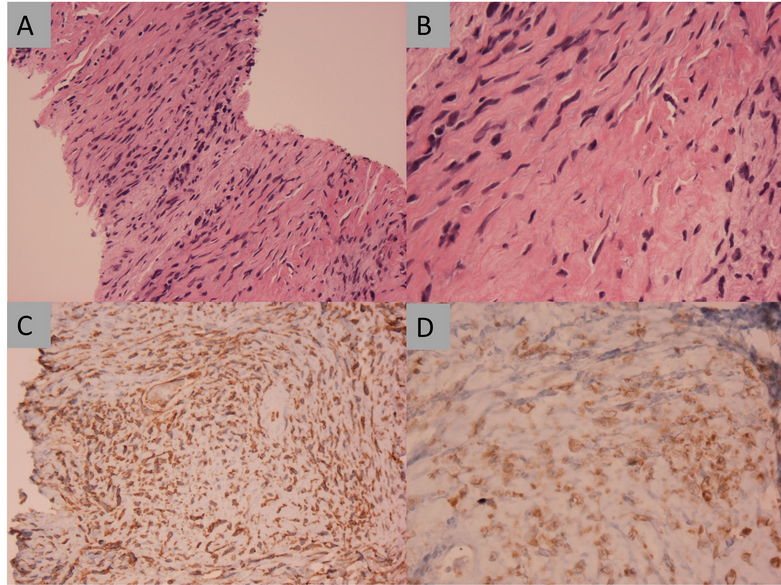
- The lung biopsy specimen with IHC analysis. Upper left (A) Hematoxylin and eosin-stained tissue (x10 magnification) shows haphazardly arranged bland-looking spindle cells admixed with collagen fibers. Upper right (B) Hematoxylin and eosin-stained tissue (x20 magnification) shows cellular variation from fibroblastic-like cells with elongated nuclei and scanty cytoplasm to epitheliod-like oval cells with abundant eosinophilic cytoplasm and round to oval, centrally located, nuclei. Lower left (C) CD34 IHC staining (x50 magnification) is positive. Lower right (D) BCL2 IHC staining (x100 magnification) is positive.
Pleural lipomas are extrapleural lesions with homogeneous fatty content that tend to occur in the upper chest along the second or third ribs. Pleural lipomas can also occasionally arise from the diaphragm. Pleural lipomas of diaphragmatic origin are predominantly found in a posterolateral location and have a 2:1 predilection for the left side. Their diagnosis is facilitated by CT, which is homogeneous and demonstrates characteristic low fat attenuation.
The vast majority of patients with malignant pleural mesothelioma (MPM) are ≥60 years and typically present decades after exposure to asbestos. Presenting symptoms are nonspecific and can include chest pain, dyspnea, cough, hoarseness, night sweats, or dysphagia. CT findings commonly associated with MPM include pleural thickening and nodularity, often involving the mediastinal pleura, pleural effusion, and contraction of a hemithorax.
Thoracic splenosis can occur in patients after left hemidiaphragmatic injury and splenic rupture and is usually an incidental finding on chest radiography. The interval between initial trauma and diagnosis of thoracic splenosis is 20 years on average. This trauma-related complication rarely requires a formal biopsy, and most patients with thoracic splenosis remain asymptomatic. When symptomatic, patients may present with pleurisy or recurrent hemoptysis. A solitary left-sided pleural-based nodule or a mass is seen on chest CT in 25% of cases, and multiple left-sided pleural-based nodules are seen in the remaining 75%. Technetium-99m sulfur colloid scintigraphy of the liver and spleen, indium 111 labeled platelets, or technetium-99m heat-damaged erythrocyte scintigraphy can establish the diagnosis of thoracic splenosis. In the appropriate clinical setting, it is important to consider thoracic splenosis in patients with pulmonary nodules with a history of thoracoabdominal trauma, as it may prevent unnecessary invasive procedures or surgery (choice D is incorrect). In such circumstances, one should not pursue a percutaneous CT-guided biopsy until thoracic splenosis has been definitely excluded by nuclear scintigraphy.1