splenic vein thrombosis and variceal bleed
- related: GI gastroenterology
- tags: #literature #GI
This patient presenting with gastrointestinal hemorrhage and isolated gastric varices in the setting of prior pancreatitis likely has splenic vein thrombosis (SVT). Most patients with SVT have a history of acute or chronic pancreatitis or pancreatic cancer. Thrombosis occurs as the splenic vein runs along the posterior surface of the pancreas and can become damaged or compressed due to pancreatic inflammation (or pancreatic masses/pseudocysts).
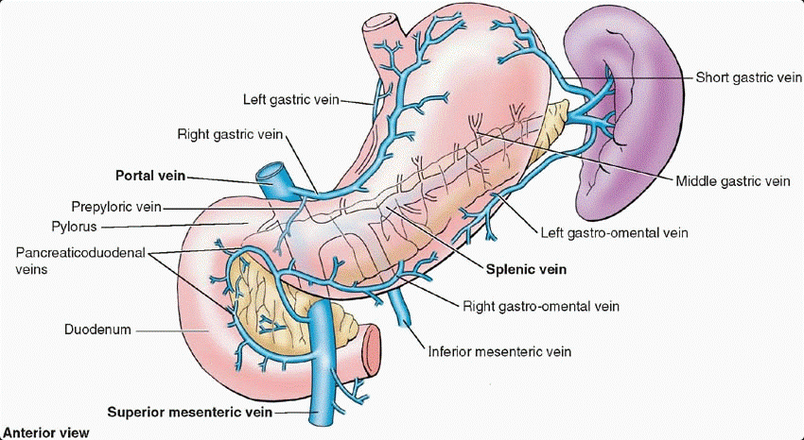
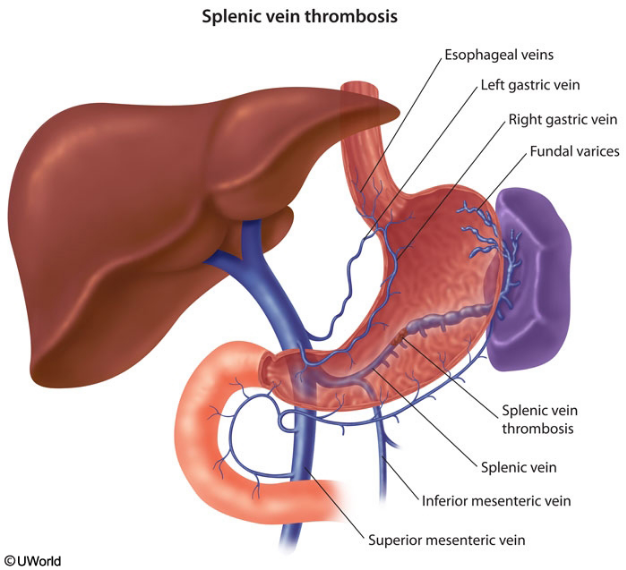
Patients with SVT are frequently asymptomatic; however, when symptoms do occur, the most common presentation is variceal bleeding. The isolated gastric varices, which are the hallmark of SVT, form when venous blood flow is redirected from the splenic vein to the collateral gastroepiploic system and short gastric veins.
Patients with chronic SVT may also develop left-sided portal hypertension (due to isolated pressure increases in the splenic portion of the portal system), ascites, and congestive splenomegaly with associated features of hypersplenism (eg, anemia, thrombocytopenia).
The diagnosis of SVT can be confirmed directly with multiple imaging modalities, including a contrast-enhanced CT scan, Doppler ultrasonography, and MRI. It can also be confirmed indirectly with esophagogastroduodenoscopy by identifying isolated gastric varices. The standard treatment for patients with SVT and gastrointestinal hemorrhage is splenectomy.
This patient presents with a GI bleed with hemodynamic instability from isolated gastric varices. Isolated gastric varices, or gastric varices without esophageal varices, have a number of potential etiologies. While many cases are due to liver dysfunction and subsequent portal hypertension, this patient does not have typical signs of liver dysfunction. Another potential etiology is splenic vein thrombosis with left-sided portal hypertension. This often occurs due to pancreatic disease due to the proximity of the pancreas and splenic vessels. Splenic vein thrombosis has been reported with pancreatitis, pancreatic masses (pseudocysts, malignancies, cystic adenomas, etc), and left gastric artery pseudoaneurysm compressing the splenic vein. The short gastric veins, which drain the fundus of the stomach, drain through the splenic vein and into the portal vein. When the splenic vein is thrombosed, venous blood from both the splenic and short gastric veins must drain back to the portal vein via collaterals, causing increased pressure in the short gastric veins, creating left-sided or sinistral portal hypertension, without right-sided portal hypertension. Recognition of this condition is important because treatment is splenectomy, which can be curative. Abdominal CT scanning with and without IV contrast demonstrated pancreatitis and splenic vein thrombosis in this patient.

The gastroduodenal artery supplies blood flow to the gastric pylorus and proximal part of the duodenum. It is often embolized to stop bleeding from duodenal ulcers on the posterior wall, which can erode into the gastroduodenal artery. However, this patient does not have any visible duodenal ulcers and does have another identified source of bleeding in the fundus of the stomach. Embolization of the gastroduodenal artery is not needed in this case and will not alleviate the bleeding.
Transjugular intrahepatic portosystemic shunt (TIPS) is often performed to alleviate increased pressure in the portal vein and decompress esophageal and gastric varices. The procedure can be lifesaving for patients with refractory variceal bleeds from classic portal hypertension. However, this patient likely has sinistral portal hypertension with normal portal vein pressures. TIPS is unlikely to alleviate the elevated pressures in the short gastric veins, which are blocked from draining by splenic vein thrombosis.
Propranolol is a nonselective β-blocking agent. Nonselective β-blockade decreases some of the mesenteric and portal pressures and prevents or delays rebleeding in patients with varices from portal hypertension. This patient does not appear to have cirrhosis, nor does he have typical portal hypertension.1234
Links to this note
-
-
related: GI gastroenterology, splenic vein thrombosis and variceal bleed
-
Chronic portal vein thrombosis is a potential complication of cirrhosis (rather than pancreatitis). Its presentation can be similar to splenic vein thrombosis and variceal bleed, but in portal vein thrombosis there is hypertension of the entire portal system with esophageal varices typically accompanying gastric varices.
-
Footnotes
-
Gotto A, Lieberman M, Pochapin M. Gastric variceal bleeding due to pancreatitis-induced splenic vein thrombosis. BMJ Case Rep. 2014;2014:pii: bcr2013201359. PubMed ↩
-
Heider TR, Azeem S, Galanko JA, et al. The natural history of pancreatitis-induced splenic vein thrombosis. Ann Surg. 2004;239(6):876-880; discussion 880-882. PubMed ↩
-
Sakorafas GH, Sarr MG, Farley DR, et al. The significance of sinistral portal hypertension complicating chronic pancreatitis. Am J Surg. 2000;179(2):129-133. PubMed ↩