spontaneous bacterial empyema SBEM is empyema without pneumonia
- related: pleural effusion
- tags: #literature #pulmonology
This patient has spontaneous bacterial empyema (SBEM), and IV antibiotics must be initiated immediately. SBEM is defined as an infection in a preexisting pleural effusion without evidence of pneumonia. Most patients with SBEM have cirrhosis and hepatic hydrothorax, though a few cases in noncirrhotic patients have been reported. In 40% of cases, SBEM occurs in the absence of spontaneous bacterial peritonitis (SBP).
The incidence of SBEM is reported to be about 15% in patients with cirrhosis and hepatic hydrothorax, though is likely underestimated due to culture collection techniques. A high Child-Pugh score, low pleural fluid protein, low pleural fluid C3 levels, and concomitant SBP have been identified as risk factors for the development of SBEM. Mortality is reported at close to 20%, with a multivariate regression analysis demonstrating a high Model for End-Stage Liver Disease sodium score, initial ICU admission, and initial antibiotic treatment failure as independent factors related to poor outcome. The source of infection may be migration of infected peritoneal fluid into the pleural space via diaphragmatic defects when SBP is present. However, since slightly less than half of the episodes are not associated with SBP, or even ascites in some cases, an alternative source may be hematogenous seeding of the pleural fluid from transient intestinal bacterial translocation. It has been shown that patients with cirrhosis and pleural effusion demonstrate low opsonic activity and complement levels in pleural fluid, and this may predispose them to the development of infection. Symptoms include dyspnea and pleuritic chest pain when restricted to the thorax, and peritoneal symptoms when associated with SBP. Fever and encephalopathy can be seen with sepsis.
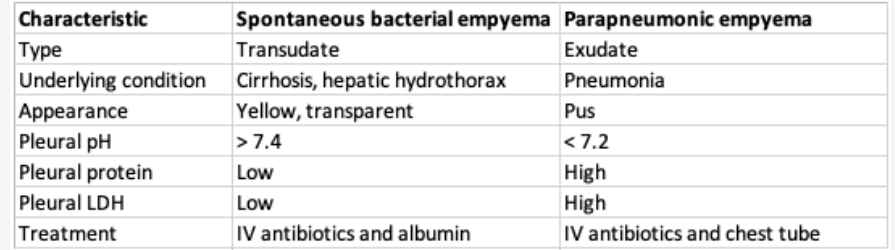
Pleural fluid in patients with SBEM typically appears yellow and transparent, and not purulent as in the case of a parapneumonic empyema (Figure 1). Pleural fluid analysis is usually transudative with normal pH and glucose and low protein consistent with a hydrothorax. SBEM is diagnosed when the pleural fluid neutrophil count is >500/μL (0.5 × 109/L), as in this case, or >250/μL (0.25 × 109/L) with a positive fluid culture. If the traditional criteria for empyema are not met, some advocate calling SBEM “spontaneous bacterial pleuritis.” When bacteria are isolated, the majority are gram negative, including Escherichia coli and Klebsiella pneumoniae.
Treatment is immediate initiation of a third-generation cephalosporin or a carbapenem when extended-spectrum β-lactamase–producing strains are possible. In contrast to treatment for a parapneumonic empyema, chest tubes are relatively contraindicated for SBEM because treatment with antibiotics alone is commonly successful and tubal drainage can lead to protein loss and electrolyte abnormalities and be a nidus for infection (choice B is incorrect). IV albumin is suggested based on the approach to SBP, though there are no specific studies for SBEM.
Transjugular intrahepatic portosystemic shunt is one way to address refractory hepatic hydrothorax and can be considered after the infection is treated in an attempt to prevent fluid recurrence (choice C is incorrect). A case report describes a patient with refractory hepatic hydrothorax who was successfully treated with IV octreotide, though this agent is more commonly used in patients with cirrhosis who have hepatorenal syndrome (choice D is incorrect). The only definitive treatment for refractory hepatic hydrothorax is liver transplantation.1