steven johnson syndrome
- related: Dermatology
- tags: #literature #icu
Causes
Diagnosis
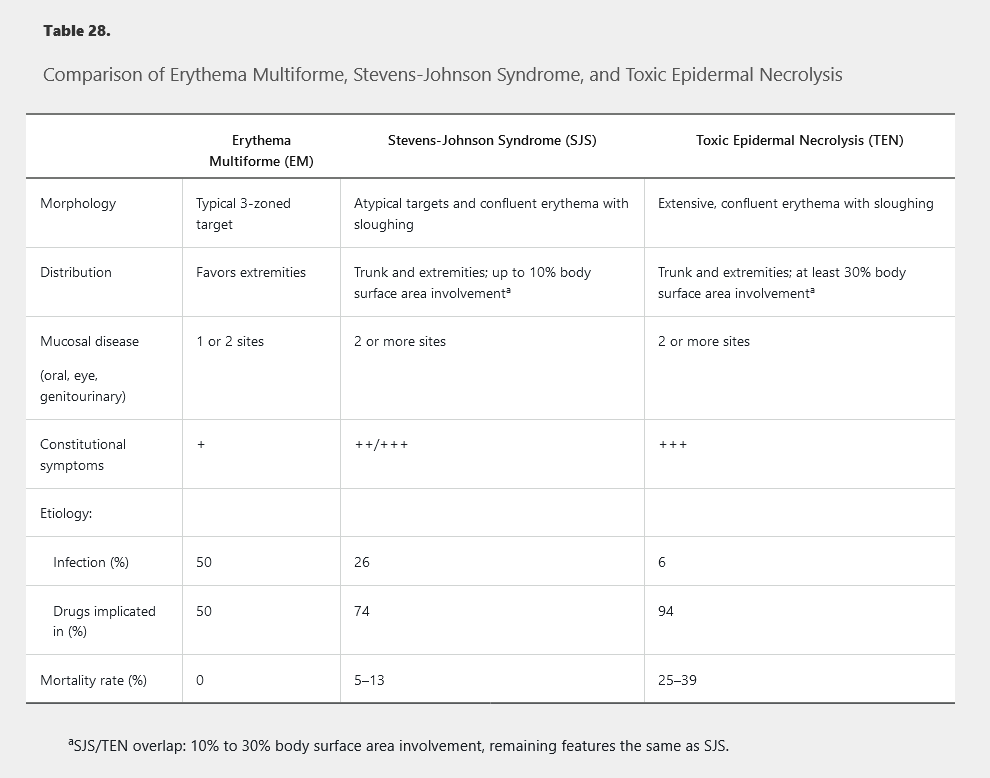
Symptoms begin usually within 1 to 3 weeks of exposure to the inciting agent. Patients may notice fever, malaise, and symptoms of upper respiratory infections followed by skin pain, grittiness or sand-like irritation of the eyes, and odynophagia. Shortly thereafter, patients develop red or purple dusky macules on the trunk that progress to vesicles, erosion, and ulceration (Figure 130). Painful erosions develop in the mouth, eyes, or genitals in as many as 95% of patients. Unlike EM’s predilection for the extremities, SJS and TEN favor the trunk and face. SJS/TEN patients may exhibit atypical targetoid macules demonstrating one or two colored rings, which can be distinguished from the three colored zones of EM. The presence of extensive epidermal sloughing and a positive Nikolsky sign further differentiate SJS/TEN from EM major (Table 28).

Swelling of the lips with vesicles on the lower lip and erosions and mucosal sloughing on the upper lip secondary to Steven-Johnson syndrome.
Systemic manifestations are common in SJS/TEN patients. All patients experience fever and malaise. Lymphadenopathy, elevated transaminase levels, and cytopenias are common. Pneumonitis, nephritis, hepatitis, and myocarditis are possible. Hypovolemia and electrolyte imbalances due to loss of the skin barrier are common.
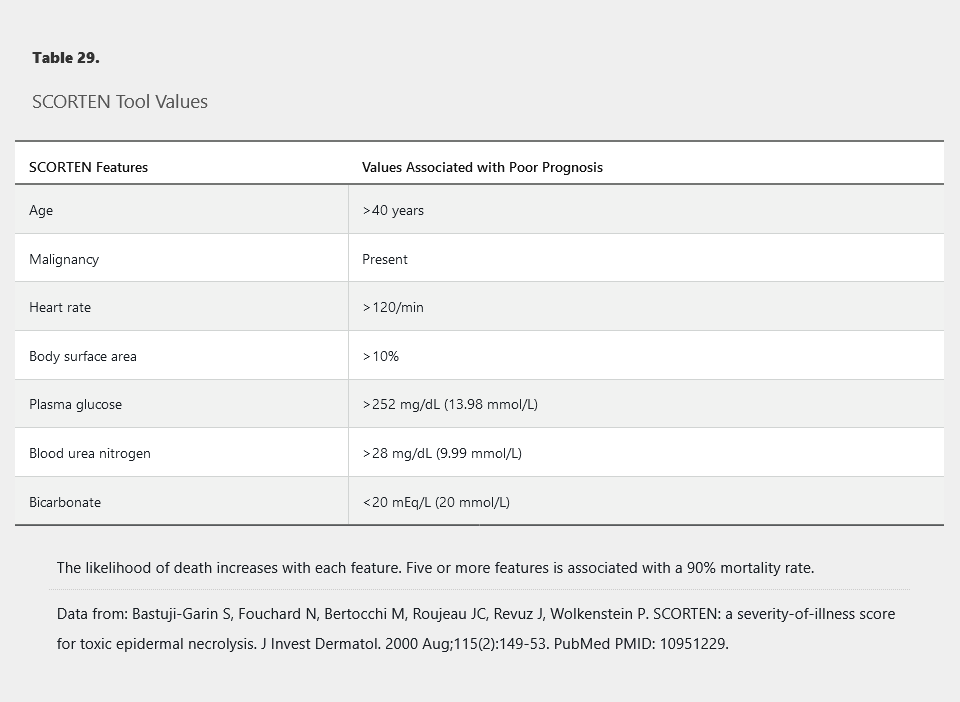
The acute phase of the disease lasts 1 to 2 weeks, and skin reepithelization may take 2 to 4 weeks. Mortality is high with 5% to 10% of SJS cases being fatal and as many as one in three patients with TEN dying from complications related to the disease. Most deaths result from secondary infection, complications of transcutaneous fluid loss, or respiratory distress. Early identification and withdrawal of the causative medication improve outcomes. The SCORTEN scale is a validated, severity-of-illness tool for TEN and SJS that can be applied early in the course of the disease. The mortality rate is directly correlated with the number of SCORTEN variables that are fulfilled (Table 29).
Body surface area is the strongest prognostic indicator in Stevens-Johnson syndrome/toxic epidermal necrosis (SJS/TEN).
Treatment of SJS/TEN is highly controversial. Intravenous glucocorticoids or intravenous immune globulins are probably the most commonly used treatments, but neither is supported by strong evidence. Supportive care in an ICU with experienced nursing staff is critical for wound care, and many patients are transferred to a burn center. Infection is a significant cause of mortality. A low threshold is recommended for performing cultures and initiation of empiric antibiotics, but use of prophylactic antibiotics is not recommended. Ophthalmologic and urologic consultations are mandatory if ocular or genital involvement is present, as destructive scarring may occur in these areas.
Links to this note
-
steven johnson syndrome causes include seizure medications
- related: steven johnson syndrome
-
phenobarbital use have increased risk for steven johnson syndrome
- This patient’s presentation is consistent with the onset of a reaction along the Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN) continuum (steven johnson syndrome). The early features of SJS/TEN include high fever, malaise, and myalgia with symptoms attributed to early mucous membrane involvement, including photophobia, conjunctival dryness and burning, orodynia, and odynophagia. Another prominent feature of early SJS/TEN is diffuse skin pain. This prodrome is typically present 1 to 3 days prior to the onset of observable cutaneous and/or mucous membrane findings. The onset of SJS/TEN is most often between 5 and 28 days from the initiation of the medication but can be seen as early as 1 to 2 days.