swimming induced pulmonary edema SIPE
- related: Pulmonology
- tags: #literature #pulmonology
This patient is most likely to have swimming-induced pulmonary edema (SIPE), also termed “immersion pulmonary edema.” A major cause of this disorder is the effect of hydrostatic forces acting on the heart and lungs (choice C is correct) during swimming.
When an adult is immersed to the neck in warm water, the hydrostatic effect of immersion causes translocation of as much as 700 mL of blood to the thorax, with an increase in cardiac size and pressures. Over time, compensatory diuresis corrects this effect. However, the stage is set for lung edemagenesis that can be clinically significant if immersion is in colder water (causing vasoconstriction of the systemic vasculature, increased left ventricular afterload, and further elevation of pulmonary microvascular pressures), vigorous exercise begins, and increased breathing effort causes swings in intrathoracic pressure.
SIPE was thought until recently to be extremely rare and limited to older individuals and those with underlying cardiac disease. Indeed, a recent study of a popular open-water swimming event in Scandinavia did find a correlation of age and cardiovascular disease with this phenomenon. However, the highest rates of SIPE, at 1% to 4%, have been seen in individuals swimming in triathlons or training for United States Navy Sea, Air, and Land Teams. Given these incidence rates and the growing popularity of large participatory sporting events, it is increasingly likely that clinicians will encounter patients with SIPE. It is not clear whether additional training can prevent SIPE, and some have observed recurrence of SIPE in highly trained individuals.
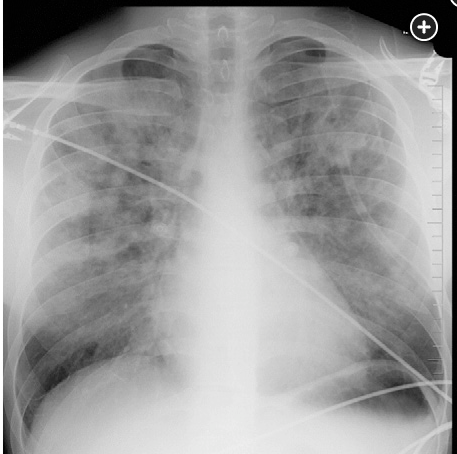
The management of SIPE is supportive and expectant. Usually removal from water and respiratory support of oxygenation will facilitate rapid recovery. This patient no longer required oxygen after 4 h in the ED, and his follow-up chest radiograph at 6 h is shown in Figure 2.
This patient’s high level of exercise prior to the event and his deterioration during immersion make undiagnosed chronic heart or lung disease unlikely (choices A and B are incorrect). There is little reason to invoke occult aspiration in an alert patient who had no sense of this happening and for whom a plausible explanation for pulmonary edema exists (choice D is incorrect).