thymoma paraneoplastic syndrome includes myasthenia gravis
- related: anterior mediastinal mass includes teratoma, thymoma, thyroid, lymphoma
- tags: #literature #pulmonology
1.thymoma::cancer: 3.myasthenia gravis most often, followed by red cell aplasia and Good syndrome::paraneoplastic syndrome associatiation
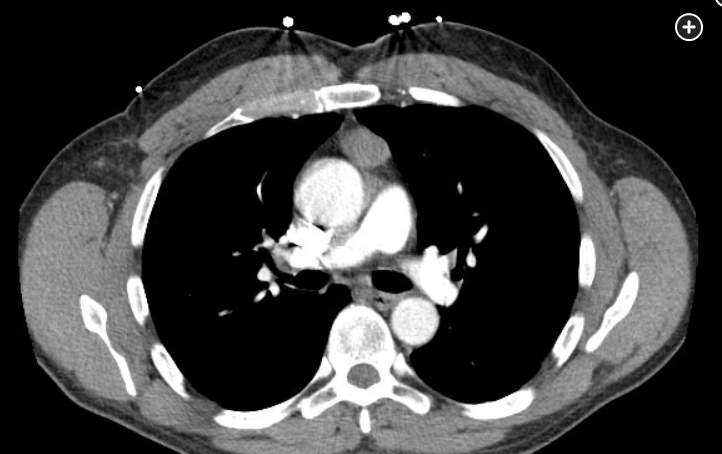
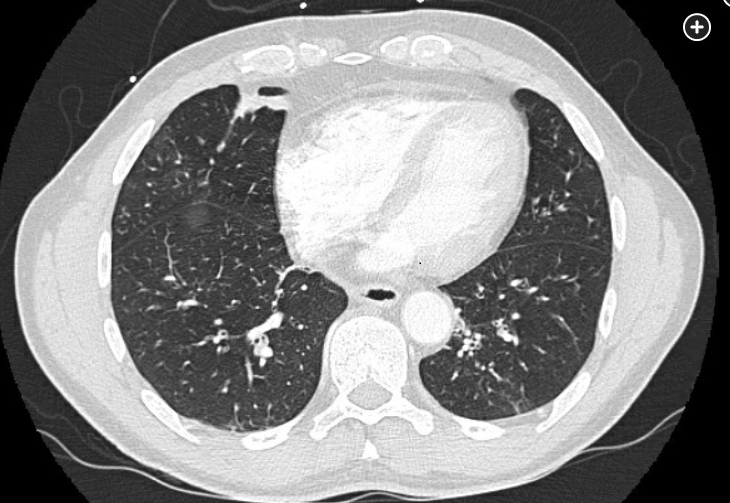
Chest CT imaging showed a smooth-bordered solid, anterior, mediastinal mass. The most common etiology of this mass is a thymoma. Myasthenia gravis is the most common paraneoplastic presentation of thymoma (choice C is correct).
The mediastinum is bordered by the thoracic inlet, the sternum, the diaphragm, the spine, and the pleural spaces. This area is divided into compartments that assist with the differential diagnosis of mediastinal masses. The anterior mediastinum is posterior to the sternum and anterior to the great vessels and pericardium. It contains the thymus and lymph nodes as well as the internal mammary arteries. The most common anterior mediastinal masses are related to the thymus (thymoma, cyst, carcinoma). Lymphoma, germ cell tumors, and thyroid tissue (substernal goiter or ectopic thyroid tissue) also lead to masses in this space.
Thymomas can present with symptoms related to their size and proximity to adjacent structures. Dyspnea, cough, chest pain, and symptoms of the superior vena cava syndrome may occur. Separately, they may present as a paraneoplastic syndrome, with symptoms unrelated to their physical impact on adjacent structures. These paraneoplastic syndromes are often autoimmune mediated.
Many paraneoplastic neurologic syndromes have been reported in connection to thymoma, the most common being myasthenia gravis. Myasthenia gravis may occur in up to 50% of patients. Usually the thymoma is at an earlier stage at the time of diagnosis than in those without myasthenia gravis (choice B is incorrect). Surgical resection (thymectomy) often leads to symptom improvement but may not lead to complete resolution (choice A is incorrect). Other paraneoplastic neurologic syndromes include polymyositis, neuromyelitis optica, sensory neuropathy, and Lambert-Eaton myasthenic syndrome.
Hematologic paraneoplastic syndromes are also commonly connected to the presence of a thymoma. Pure red cell aplasia is the most common, present in up to 15% of patients. This presentation is more common in older women and tumors with spindle cell morphology. Surgical resection (thymectomy) is recommended but infrequently leads to remission. Other hematologic paraneoplastic syndromes have been reported, including hemolytic anemia and agranulocytosis.
Thymoma has also been associated with acquired hypogammaglobulinemia (Good syndrome) (choice D is incorrect) and dermatologic, endocrine, GI, and rheumatologic manifestations. There have been a few case reports of diffuse panbronchiolitis (without hypogammaglobulinemia) in association with thymomas. The patient described in this question had several features of diffuse panbronchiolitis, including a persistent cough with sputum production and dyspnea, symptoms and imaging suggesting chronic sinusitis, chest imaging showing diffuse centrilobular micronodules and airway thickening (Figure 2), obstructive lung function testing, and crackles on exam. A biopsy was not performed. Immunoglobulin levels were normal. Given this presentation, azithromycin was started at 500 mg/day. One month later, his symptoms and pulmonary function testing improved (FEV1 of 1.45 L, 43% predicted postbronchodilator and a mildly reduced diffusing capacity (60% predicted) at baseline; FEV1 75% predicted and diffusing capacity 83% predicted while receiving azithromycin). He then underwent a thymectomy, and the azithromycin was discontinued. His symptoms had resolved, imaging improved, and pulmonary function testing normalized (FEV1 88% predicted) (Figure 3).1