toxic shock syndrome from nasal packing
- related: necrotizing infections
- tags: #literature #id
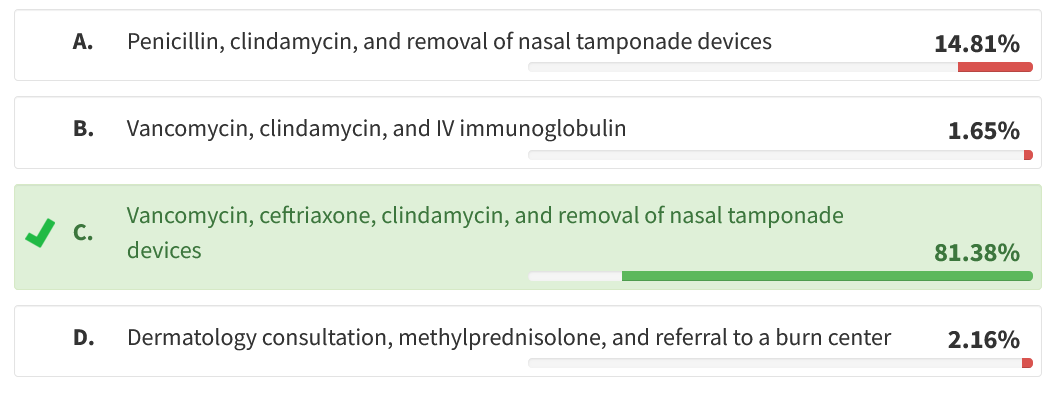
This patient has staphylococcal toxic shock syndrome, likely related to the nasal tamponade devices (“nasal tampons,” marketed under multiple brand names). Given the prevalence of methicillin-resistant Staphylococcus aureus (MRSA), especially among patients with frequent exposure to the hospital environment, an empiric treatment strategy for staphylococcal toxic shock must include an agent, such as vancomycin, that is active against MRSA. For source control, removal of the tamponade balloons is necessary. Whether additional source control would be required is unlikely but not impossible. Toxic shock syndromes generally are considered to result from a toxin (hence “toxic”) elaborated by the infecting bacteria, which elicit a response from the host. In the case of staphylococcal toxic shock, the toxin is the unimaginatively named toxic shock syndrome toxin 1, which, as a superantigen, binds to T-cell receptors (generally major histocompatibility complex class II) that then activate an extravagant immune response, disproportionate to the degree of infection and mediated by proinflammatory cytokines. These toxins are part of the S aureus pathogenicity island; together they seem to persist by token of inducing immune dysregulation, which ultimately favors greater reproductive success for the bacteria. While penicillin, clindamycin, and removal of nasal tamponade devices would be appropriate if the pathogen were a Streptococcus species, the risk of MRSA mandates inclusion of an agent effective against MRSA. Vancomycin, clindamycin, and IV immunoglobulin do not achieve source control. While drug reaction with eosinophilia and systemic symptoms syndrome is an important problem encountered in the ICU and can cause organ failure and even hypotension, this is usually accompanied by eosinophilia; in this case, staphylococcal toxic shock is more likely.123
A 66-year-old woman with acute myeloid leukemia is recovering from human leukocyte antigen-matched bone marrow transplant. Moderate cytopenias have persisted. Her absolute neutrophil count is 1,200/μL (1.20 × 109/L), hemoglobin is 8 g/dL (80 g/L), and platelet count is 26 × 103/μL (26 × 109/L). She presents to the ED with severe epistaxis. She is intubated, with substantial difficulty, for airway protection in the ED; bilateral nares are packed with nasal tamponade devices. The epistaxis improves, but the patient develops respiratory failure and is slow to awaken. She is treated with ciprofloxacin 400 mg IV every 12 h. On hospital day 4, she develops fever, a diffuse blanching rash, and hypotension that persists despite 5 L of balanced crystalloid infusion and initiation of norepinephrine infusion. Her platelet count has dropped to 12 × 103/μL (12 × 109/L). On the basis of this information, the optimal early treatment of this patient includes which of the following?
Links to this note
Footnotes
-
Kim D, Hong JS, Yoon EJ, et al. Toxic shock syndrome toxin 1-producing methicillin-resistant Staphylococcus aureus of clonal complex 5, the New York/Japan epidemic clone, causing a high early-mortality rate in patients with bloodstream infections. Antimicrob Agents Chemother. 2019;63(11):pii: e01362-19. PubMed ↩
-
Spaulding AR, Salgado-Pabón W, Kohler PL, et al. Staphylococcal and streptococcal superantigen exotoxins. Clin Microbiol Rev. 2013;26(3):422-447. PubMed ↩