use cardiac MRI to diagnose myocarditis
- related: Cardiology
- tags: #literature #cardiology
From the history and clinical presentation provided, this patient is highly likely to have acute myocarditis, producing congestive heart failure and cardiogenic pulmonary edema as causes of shortness of breath and hypoxemia. Cardiac MRI after gadolinium enhancement would be an appropriate imaging modality to support this diagnosis.
Myocarditis is an inflammatory disorder of the myocardium that in the past often required a histologic diagnosis after myocardial biopsy. In recent decades, diagnostic criteria have shifted to noninvasive testing, including highly sensitive troponin measurement and cardiac MRI, reserving biopsy for more diagnostically ambiguous cases. MRI criteria for diagnosing myocarditis include intense signal after gadolinium enhancement, which results from hyperemia; increased myocardial T2 relaxation time or intensity associated with myocardial edema; and late gadolinium enhancement, indicating necrosis or fibrosis (Figure 3).
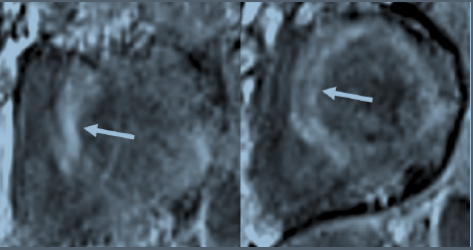
Late gadolinium-enhanced images of short-axis views of the left ventricle. Arrows show diffuse patchy areas of enhancement consistent with myocardial necrosis and/or fibrosis. Images were obtained from a patient with acute myocarditis associated with COVID-19 pneumonia.
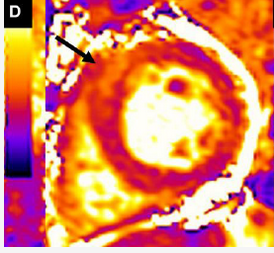
Short-axis MRI scan of left ventricle after gadolinium enhancement. T2 mapping of this slice shows heterogeneous myocardial edema (arrow). This image was obtained from a patient with acute myocarditis complicating COVID-19 pneumonitis.
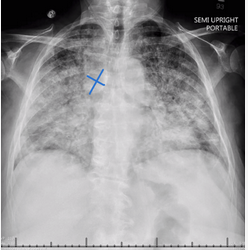
Chest radiograph with bilateral diffuse infiltrates, cardiac enlargement, and extremely enlarged azygos vein (blue markers), signaling venous hypertension typical of cardiogenic pulmonary edema.
The causes of myocarditis are often divided into noninfectious and infectious causes. Noninfectious causes include immune stimulation (sarcoidosis, vaccines, or cancer therapies such as immune checkpoint inhibitors) and exposure to toxins and drugs. A wide variety of autoimmune disorders must be considered as potential causes including hypersensitivity states, eosinophilic granulomatosis and polyangiitis, and idiopathic hypereosinophilic syndrome (Löffler’s endocarditis). Viruses are the most common cause of infectious myocarditis, but certain parasitic infections should be considered in the appropriate context. During the early COVID-19 pandemic, the incidence of definite or probable myocarditis was estimated as 2.4 cases per 1,000 patients hospitalized, likely higher than the background incidence of this cardiac injury. There appears to be a higher incidence in male patients. Direct viral injury to myocytes and/or immune processes triggered by the initial infection are presumed mechanisms of injury. Myocarditis has also been seen in surveillance studies of individuals receiving messenger RNA COVID-19 vaccines, with an estimated incidence of 1 case per 100,000 vaccine recipients. These data indicate that the risk of myocarditis is higher from the viral infection itself than from the vaccination to prevent it.
The clinical presentation of myocarditis varies widely, with chest pain common early and then a wide range of cardiac functional states, ranging from well-preserved ventricular function to severe cardiogenic shock. Arrhythmias and conduction disturbances are common with more severe ventricular dysfunction. ECG changes in general are nonspecific, with tachycardia and nonspecific ST-T wave changes often present (as in this patient). This patient’s chest radiograph was typical of cardiogenic pulmonary edema, with bilateral diffuse infiltrates, cardiac enlargement, Kerley B lines, and an extremely large azygos vein signaling venous hypertension (see Figure 4, with blue markers showing azygos vein). Echocardiography is useful to determine the degree of ventricular impairment, which was severe in this patient.
Treatment of myocarditis includes management of arrhythmias and heart failure with the usual tools, as well as condition-specific therapy when the most likely cause(s) of a particular instance of myocarditis are identified. Empiric treatment with IV glucocorticoids is advocated by many for patients with cardiogenic shock, advanced heart failure, or arrhythmias. Many experts recommend myocardial biopsy if corticosteroids are to be administered for a prolonged period.
While some data suggest patients with active or recent COVID-19 infection have an increased risk for venous thromboembolism, the findings in this patient do not point to a primary insult to the pulmonary circulation and right heart, and there would be little reason to pursue a diagnosis of pulmonary embolization. Repeat PCR testing on bronchoscopic specimens would have low yield after negative PCR swab (although the sensitivity of this testing is not above 90%), would not directly explain the cause of myocardial dysfunction if positive, and would require an invasive procedure with risks; moreover, many cases of COVID-19-associated myocardial disease progress after viral replication in the respiratory tract has subsided. This patient’s cardiogenic pulmonary edema more than adequately explains this patient’s hypoxemia, and exploring intracardiac shunting is not a high-yield endeavor.123456
Links to this note
Footnotes
-
Ammirati E, Frigerio M, Adler ED, et al. Management of acute myocarditis and chronic inflammatory cardiomyopathy: an expert consensus document. Circ Heart Fail. 2020;13(11):e007405. PubMed ↩
-
Basso C. Myocarditis. N Engl J Med. 2022;387(16):1488-1500. PubMed ↩
-
Ferreira VM, Schulz-Menger J, Holmvang G, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018;72(24):3158-3176. PubMed ↩
-
Witberg G, Barda N, Hoss S, et al. Myocarditis after Covid-19 vaccination in a large health care organization. N Engl J Med. 2021;385(23):2132-2139. PubMed ↩
-
Lasica R, Djukanovic L, Savic L, et al. Update on myocarditis: from etiology and clinical picture to modern diagnostics and methods of treatment. Diagnostics (Basel). 2023;13(19):3073. PubMed ↩