use double sequential external defib in persistent vfib arrest
- related: cardiac arrythmia
- tags: #literature #icu #cardiology
The stem describes a patient with ischemic cardiomyopathy who has a V-fib arrest in the ICU. CPR is initiated, and the patient receives advanced cardiac life support according to the American Heart Association guidelines. However, his V-fib has been refractory to standard defibrillation attempts. Are there alternative strategies that we can use?
In a cluster randomized trial (DOSE VF), Cheskes and coworkers compared two novel defibrillation strategies, one called “double sequential external defibrillation” (DSED) and the other “vector-change” (VC) defibrillation, to standard defibrillation in adult patients experiencing out-of-hospital V-fib refractory to three external shocks. Survival to hospital discharge was 30.4% in the DSED group, 21.7% in the VC group, and 13.3% in the standard defibrillation group. DSED but not VC was associated with a significantly higher likelihood of a patient having a good neurological outcome compared with outcomes with standard defibrillation.
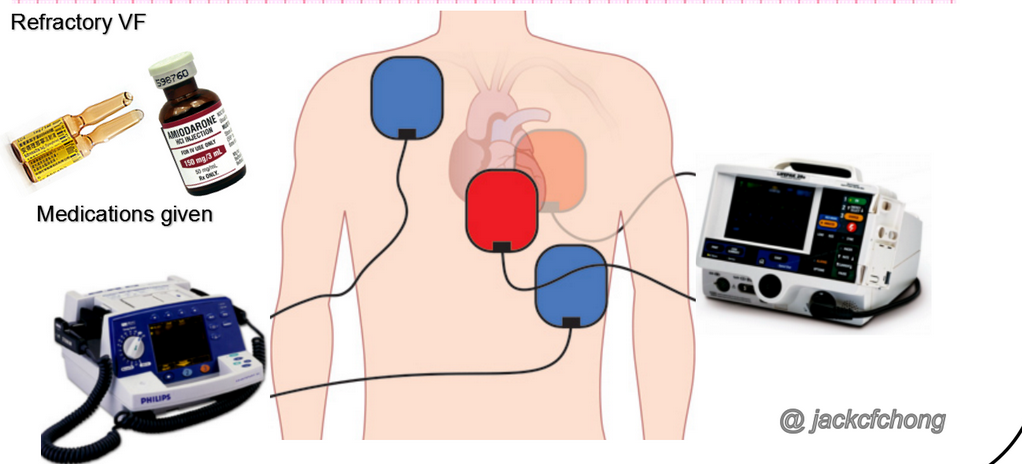
DSED uses two separate defibrillators along two axes delivering maximum energy fired by one operator in rapid sequence: One anterior-lateral is fired first, and a second anterior-posterior is fired less than 1 s later.
Cardiologists have used DSED for decades to manage refractory V-fib in the electrophysiology laboratory, but the DOSE VF trial now provides evidence of its effectiveness in patient populations outside of the cardiology suite (choice C is correct). Although the precise mechanism by which DSED works is unknown, it is theorized that more myocytes are able to be defibrillated in this mode than with standard defibrillation, perhaps because either the first shock lowers the defibrillation threshold of the remaining myocytes or the combination of the first and second shocks just delivers more total power to the myocardium. A third possibility is that the two shocks are simply delivered along different vectors.
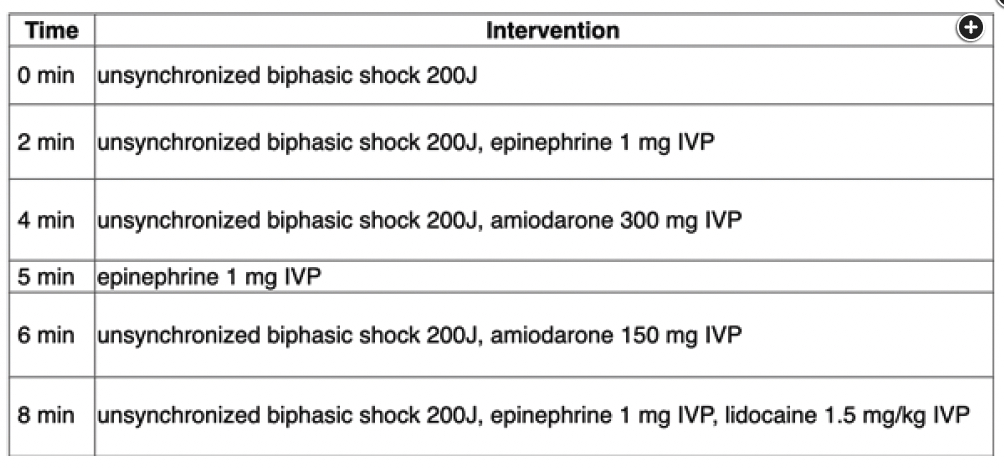
Lidocaine is a class IB Vaughan-Williams antiarrhythmic, but amiodarone is class III. Both drugs were studied in a large double-blind, randomized placebo-controlled clinical trial in patients experiencing out-of-hospital cardiac arrest. Neither drug was significantly better than placebo at improving survival to hospital discharge. That said, a least two meta-analyses have suggested that both drugs may be effective, with an OR for survival of approximately 2 for amiodarone and 1.5 for lidocaine. Furthermore, both drugs are still advocated by the American Heart Association for refractory V-fib. In any event, this patient has received the maximum recommended doses and remains in V-fib (choice A is incorrect).
Sotalol is a class II-III antiarrhythmic that has β-blocker activity, decreases atrioventricular nodal conduction, and prolongs atrial and ventricular action potentials. It is an effective antiarrhythmic for the maintenance of sinus rhythm in patients with atrial fibrillation and atrial flutter. It can also be used to suppress malignant ventricular arrhythmias. It has not been adequately studied in cardiac arrest due to V-fib and would theoretically be contraindicated because of its β-blocking effects (choice B is incorrect).
The decision to halt resuscitation attempts is a complicated one. There are several reasons to consider continuing resuscitation attempts in this case. First, this patient appears to have the potential for a good neurological outcome as evidenced by his reactions during CPR, which include arm and leg movement and grimacing. Second, his end-tidal CO2 measurement of 25 mm Hg portends a better prognosis. Finally, on the basis of the information provided, he is likely a candidate for advanced interventions such as revascularization or transplant. For these reasons, an extended resuscitation attempt is warranted (choice D is incorrect).12345
A 47-year-old patient with newly diagnosed ischemic cardiomyopathy is admitted to the ICU with a non-ST segment elevation myocardial infarction. He receives IV morphine, which relieves his chest pain. His potassium and magnesium levels are normal. During transfer to his ICU bed, he has sudden loss of consciousness. His monitor shows ventricular fibrillation (V-fib). Because he is already wearing defibrillation pads, he is given an immediate 200-J shock from an automated external defibrillator and chest compressions and rescue breathing are initiated by his bedside nurses. The quality of the chest compressions is thought to be excellent as judged by a compression rate of 110/min, a compression depth of 5 cm, an end-tidal CO2 of approximately 25 mm Hg, and spontaneous movement of the patient’s arms during CPR. A summary of his code blue worksheet is shown in Figure 1. In spite of the above, he remains in V-fib.
What intervention would you recommend now?
Links to this note
Footnotes
-
Cheskes S, Verbeek PR, Drennan IR, et al. Defibrillation strategies for refractory ventricular fibrillation. N Engl J Med. 2022;387(21):1947-1956. PubMed ↩
-
Kudenchuk PJ, Brown SP, Daya M, et al; Resuscitation Outcomes Consortium Investigators. Amiodarone, lidocaine, or placebo in out-of-hospital cardiac arrest. N Engl J Med. 2016;374(18):1711-1722. PubMed ↩
-
Sanfilippo F, Corredor C, Santonocito C, et al. Amiodarone or lidocaine for cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2016;107:31-37. PubMed ↩
-
Wang Q, Lin Z, Chen H, et al. Comparison the efficacy of amiodarone and lidocaine for cardiac arrest: a network meta-analysis. Medicine (Baltimore). 2023;102(15):e33195. PubMed ↩