use of esophageal manometry to guide PEEP
- related: ICU intensive care unit
- tags: #literature #icu
The distending pressure or transmural pressure across the lung is known as . can be calculated using the simple formula that represents all transmural pressures, which is the pressure inside the system minus the pressure outside the system. For the lung under static conditions, this translates to PL = Paw − Ppl, where Paw is the airway pressure and Ppl is the pleural pressure.
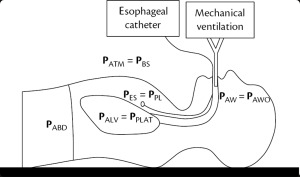
Esophageal manometry is a technique used to indirectly measure or estimate pleural pressure using esophageal pressure (Pes) and has been used to guide mechanical ventilation using the principles of PL.
When PL is negative at the end of expiration (when Paw = PEEPtotal), this represents a condition in which the pressure outside the system (Ppl) is greater than the pressure inside the system (Paw). This results in atelectasis in the area of the lung for which the PL is negative and also may predispose the patient to ventilator-induced lung injury through atelectrauma, or cyclic atelectasis. Thus, one goal of using Pes to guide mechanical ventilation is to minimize dependent atelectasis and atelectrauma by achieving a positive PL (PL > 0 cm H2O) at end expiration by increasing applied PEEP (choice C is correct; choice A is incorrect).
A second goal of using PL and esophageal manometry to guide mechanical ventilation is to minimize overdistension at end inspiration. While the precise limit of a safe end-inspiratory PL has not been definitively established, the generally accepted goal is below 20 to 25 cm H2O. This patient has an end-inspiratory PL of 12 cm H2O, which is well below the threshold considered to represent overdistension. Thus, although the end-inspiratory plateau pressure in this patient is measured at 36 cm H2O, the PL measurements suggest that this airway opening pressure measurement is likely due to decreased compliance of the chest wall and/or abdomen instead of overdistension of the lung, so decreasing the tidal volume below the recommended 6 cc per mL of predicted body weight would not be indicated (choice B is incorrect). Furthermore, increasing the tidal volume would not mitigate the atelectrauma that is due to a negative transpulmonary pressure at the end of expiration (choice D is incorrect).
The above rationale for and description of using PL to guide mechanical ventilation is grounded in physiological principles. In clinical trials based on several of these principles, however, investigators have found mixed results. In the 2008 EPVent trial, investigators found that a Pes-guided PEEP strategy improved the physiological targets of oxygenation and lung compliance compared with a control group. However, the follow-up EPVent-2 study failed to demonstrate an improvement in the patient-centered outcomes of mortality or ventilator-free days for patients who received PEEP titrated by Pes compared with a control group. It is important to note, however, that control patients in EPVent were ventilated with a lower empiric PEEP table compared with control patients in EPVent-2, which may partially explain the discrepant results.123456
A 51-year-old woman with class III obesity (BMI, 44 kg/m2) develops ARDS after an aspiration event. She is intubated and mechanically ventilated with volume assist-control ventilation. Her current ventilator settings are FiO2 of 1.0, tidal volume of 6 mL/kg predicted body weight, PEEP of 8 cm H2O, and set rate of 35/min. The peak pressure on the ventilator is 41 cm H2O, and plateau pressure is 36 cm H2O. An arterial blood gas demonstrates a pH of 7.20, PCO2 of 55 mm Hg, and PO2 of 52 mm Hg.
An esophageal balloon is placed to assist in the ventilator management. On her current ventilator settings, at end inspiration, her transpulmonary pressure (PL) is calculated to be 12 cm H2O. At end expiration, her PL is calculated to be -4 cm H2O.
Which of the following choices would reduce the risk of atelectrauma in this patient?
Links to this note
Footnotes
-
Beitler JR, Sarge T, Banner-Goodspeed VM, et al; EPVent-2 Study Group. Effect of titrating positive end-expiratory pressure (PEEP) with an esophageal pressure-guided strategy vs an empirical high PEEP-Fio2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2019;321(9):846-857. PubMed ↩
-
Mauri T, Yoshida T, Bellani G, et al; PLeUral pressure working Group (PLUG—Acute Respiratory Failure section of the European Society of Intensive Care Medicine). Esophageal and transpulmonary pressure in the clinical setting: meaning, usefulness and perspectives. Intensive Care Med. 2016;42(9):1360-1373. PubMed ↩
-
Talmor D, Sarge T, Malhotra A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med. 2008;359(20):2095-2104. PubMed ↩
-
Yoshida T, Amato MBP, Grieco DL, et al. Esophageal manometry and regional transpulmonary pressure in lung injury. Am J Respir Crit Care Med. 2018;197(8):1018-1026. PubMed ↩
-
Yoshida T, Grieco DL, Brochard L. Guiding ventilation with transpulmonary pressure. Intensive Care Med. 2019;45(4):535-538. PubMed ↩